How to build (more) peer mentor programs in kidney care
What works and what we can learn from cancer care, behavioral & mental health
A critical gap exists in the support system for individuals living with kidney disease and those who care for them.
Being diagnosed with kidney disease (CKD) or experiencing kidney failure (ESKD) often marks the beginning of a challenging and isolating journey. Emotional and mental well-being play pivotal roles in shaping a patient's overall quality of life and health outcomes. The prevalence of depression is 3 to 4 times higher among CKD and ESRD patients compared to the general population, making psycho-social support an integral part of "whole person" kidney care.1
Enter peer mentoring programs. These initiatives have proven effective in improving clinical, emotional, and economic outcomes across a range of conditions and patient populations. Peer mentors are individuals who have been through similar challenges, offering patients a relatable and trustworthy source of support. It's a powerful way to extend a helping hand to those in need, from those who've walked in their shoes.
So, why aren't we seeing more of them in kidney care? The short answer is: there’s still work to be done around health economics and outcomes that should (in theory) increase uptake in kidney care settings. However, there may be a path forward in the nearer term if an intrepid, innovative care delivery company wants to take a page out of another sector's playbook.
In today's exploration, we delve into the potential of peer-to-peer (P2P) mentor programs, their role in overcoming access barriers, and the (in)valuable lessons we can glean from successful programs in other areas.
IN THIS ISSUE
InquisitHealth’s remote, tech-enabled peer mentor programs
Insights from designing & delivering programs in kidney care
Lessons on scaling P2P from cancer & behavioral health care
Why it matters and what’s next in this space
1. Delivering remote, tech-enabled peer mentor programs with InquisitHealth



InquisitHealth is a remote, technology-enabled peer mentoring company that delivers chronic disease management longitudinally and one-on-one to patients, through telephonic and smartphone outreach in English and Spanish. Workforce: The company employs Peers — community health workers paired with patients based on their shared cultural background, clinical condition, and lived experience — to help engage patients, address social needs, and improve chronic disease management.
Research: The InquisitHealth team has strong clinical research chops with over $2.4 million in NIH-funded work to date. They recently launched an NIH-funded trial to expand their Mentor1to1™ platform to deliver a physical activity program for breast cancer survivors. Another study delivered a remote P2P intervention in a safety net hospital in New York and showed improved diabetes outcomes and social determinants among diverse patients.
Results: A few notable outcomes from past programs include:
10+ point increase in patients’ patient activation score (PAM) for participants in the National Kidney Foundation’s NKF PEERs program
1.7 point HbA1c decrease for patients at Montefiore in New York
10+ point systolic BP drop for members of the Massachusetts 1199SEIU Fund
Milestones: As of 2018, the company had raised $4.2 million, including non-dilutive NIH grants and seed checks from Dreamit and Hudson River Capital Partners.
2. What we know about current programs in kidney care
A number of grassroots peer mentor programs have been launched by non-profits with national reach like the NKF and AAKP. The ESRD Networks offer a toolkit designed to help dialysis clinics implement their own peer mentor programs from the ground up. But we still have a ways to go and adoption remains low.
Studies like PEER-HD aim to better understand the potential impacts of peer-driven programs on downstream adverse events like ED visits and hospitalizations.
Our personal experiences in two programs in particular are highlighted below, including Lyfebulb (where
is a Transplant Community Manager) and ReMend (where runs a program in partnership with Balboa Nephrology).Lyfebulb is an innovation accelerator that bridges the gap between patient communities and the healthcare industry by working directly with patients and care partners to generate insights and build new solutions to reduce the burden of living with chronic disease.Communities: Lyfebulb partners with industry sponsors to source user-driven innovation from 12 patient Communities, including CKD, transplantation, diabetes, cancer, and others. In early 2021, Lyfebulb launched the first digital venue, TransplantLyfe, for patients with organ transplants (and their care partners) to connect and learn from each other, access expert educational resources, and innovate.
Alex’s POV 🗨️:
“As a community manager with TransplantLyfe one of my roles is to encourage the online patient community to feel that they can bring their experience dealing with a Kidney transplant. I have also been tasked with helping to find new ways to partner with orgs like AAKP and NKF.
In our online forums we get a variety of different patient experiences and I think with Lyfebulb their online forum support has given patients a chance to share insight on the journey and in turn give others the confidence to deal with CKD.”
Lyfebulb also has an online health tracker and a section that discusses clinical trials. This platform and webinars really give patients the opportunity to feel heard.”
ReMend is a group of volunteers who have experienced kidney disease as patients themselves and are focused on giving hope to people on their kidney journey.Community: ReMend just launched a no-cost, online kidney community that’s open to anyone currently receiving dialysis. It’s a first-come, first-served open forum for groups of 6 to 8 patients with guidance from ReMend’s mentors. You can register for an upcoming event online— the next sessions are on November 9 and 15.
Conversations: In addition to the one-on-one and group group sessions, ReMend also runs a series of free, monthly webinars called Kidney Conversations. These offer candid, educational discussions featuring health experts and mentors who share their own patient perspectives.
Kiku’s POV 🗨️:
“One of the features of ReMend has been "mentor matching .This feature was something we were able to manage for many years - where we matched patients with mentors who had something in common, whether it was age, modality, hobbies, family life, etc.
We've realized that mainly, people just want to be heard - and heard by folks who understand what they're going through. Of course, some patients prefer specifics i.e., age or gender, when working with a mentor, but it hasn't proven to be a situation within the past year.”
3. What we can learn from the broader chronic care market
Two companies outside of kidney care stood out in our search for evidence-based, peer-driven support programs. From the looks of it, to deliver truly comprehensive, whole-person care for those who need it most, providers will need to have a peer-driven engagement strategy. Here are two examples of how that might look as new and existing programs scale and find their way into CKD and ESRD.
Jasper Health is a leading digital oncology support company dedicated to transforming the cancer care experience for patients and their caregivers. Community: Earlier this year the team announced the launch of a proprietary peer-to-peer member community network along with a coalition of non-profit cancer support organizations, which is now available to Jasper’s 17,000+ members.2 So far, the company has seen 100 percent member satisfaction with Jasper Care Coaching.
Milestones: Since spinning out of Redesign Health, Jasper has landed a string of impressive partnerships including MSK Direct, Evernorth, Covet Health, Wellnecity, CancerX, Walgreens, and a $25 million Series A funding round led by General Catalyst with participation from 7wireVentures, Redesign, and others.
Firsthand is changing the way individuals struggling with serious mental illness (SMI) engage with the healthcare ecosystem, focusing on delivering real outcomes for a population that has historically been underserved, stigmatized, and deprioritized. 



Care Model: Firsthand uses a peer-support model to help patients with SMI access care. All its peer-support specialists, called firsthand guides, have lived experience with SMI and are trained to engage with a patient at home. Our thanks to senior firsthand guide Tesla Metzger who shared team celebration photos from World Peer Support Day last week.
Tailwinds: According to the CDC, only 64% of adults with SMI received mental health treatment in the past year. In June the Substance Abuse and Mental Health Services Administration (SAMHSA) released new national model standards for peer support certification focused on the behavioral health workforce.3 The program’s goal is to:
“…speed up the universal adoption, recognition and integration of the peer mental health workforce across the country.”
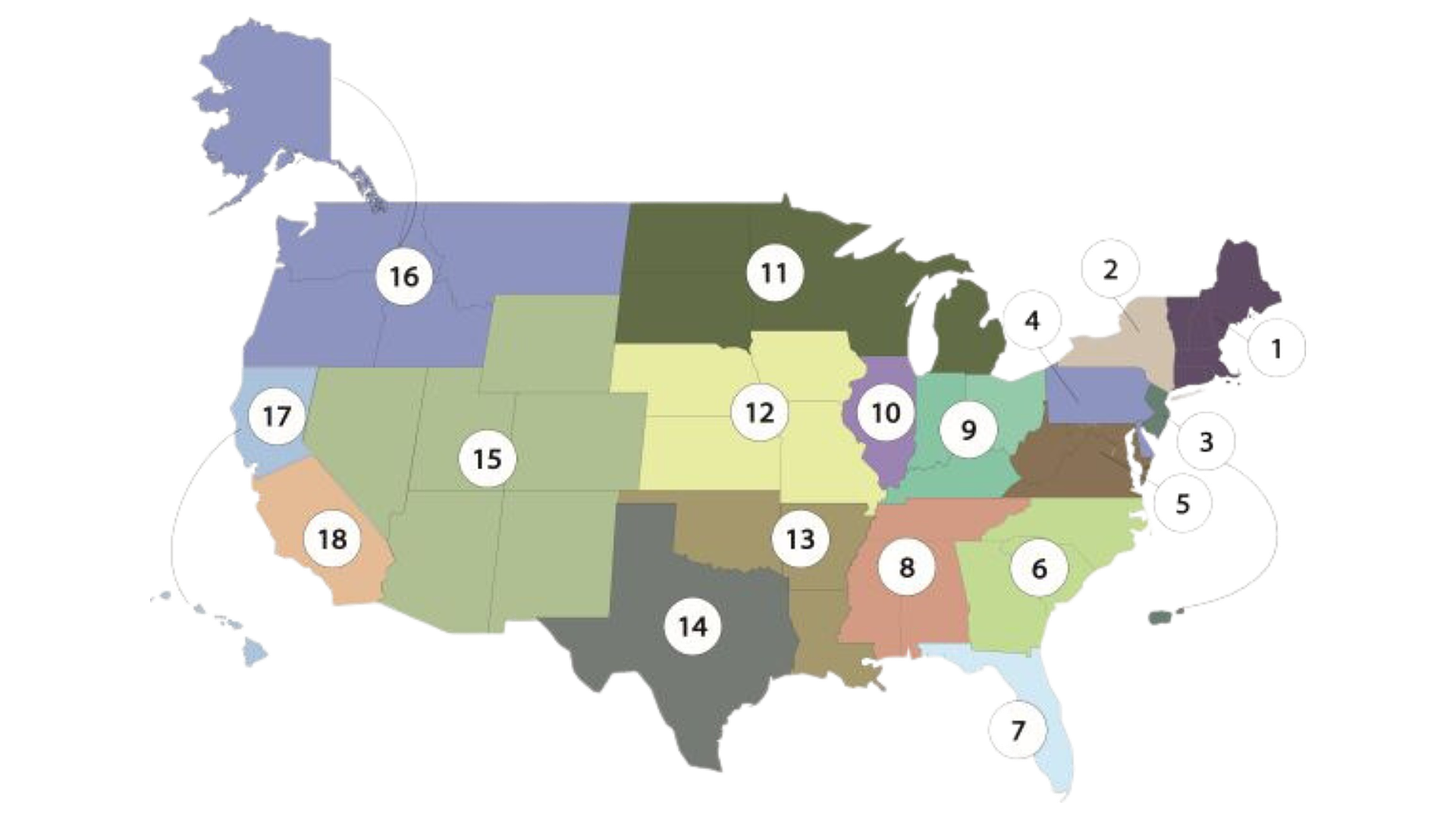
Milestones: firsthand currently supports communities in 14 cities across Florida, Ohio and Tennessee. The team announced it had raised $28 million from investors including GV (fka Google Ventures) earlier this year, bringing the total capital raised to just under $43 million.
Why It Matters
A few weeks ago we talked about the continued growth of value-based kidney care, where the 3 companies mentioned now manage over 375,000 lives and $8 billion in spend. This growing trend is one of three key reasons why we expect to see more peer programs launched over the next 3 to 5 years in ESRD settings. Others include:
Care is local. In healthcare, local factors significantly influence patient experiences and outcomes. Recall from last week, 240,000 people are living with ESRD in rural America, where access to care is limited. Peer mentoring, rooted in communities, provides essential support, connecting patients with empathetic guides who understand their local realities and personal health concerns.
Change is hard. One of the greatest challenges (and cost drivers) in healthcare today is non-adherence.4 Making changes to anyone’s lifestyle, especially big changes that include nutrition, medications, or even the use of a new app or device, can seem impossible. When you consider how daunting a chronic care diagnosis can be, or the disconnect that comes from getting a early stage CKD diagnosis without experiencing any symptoms, dissonance ensues. It helps to have someone like us, in our community and on our team, to get us to where we need to be.
What’s Next
While the potential for peer mentoring in CKD and ESRD is undeniable, the road ahead encounters a familiar challenge: buy-in. Who will tip the scales to make that happen in kidney care? As it is, we struggle to arm patients and providers with the knowledge, skills and confidence they need to navigate the disease.
No matter how this plays out, the adoption of peer mentoring will require buy-in from patients, providers, and systems at every level. Who knows, maybe it will hitch a ride on the rocketship that is value-based kidney care, fast-tracking a tech-enabled future state where peers are seamlessly integrated into the multidisciplinary, personalized care experience.
In the meantime, we remain committed to building, testing, iterating and supporting peer programs within our respective communities. We hope these insights shared today bring you closer to introducing peer support to a community near you.
Further reading
We thought we’d wrap today’s Signal with a few stories and articles worth reading. We hope you enjoy and we’ll see you again for next week’s Signal.
Empathy and Resilience: Meet Asa, Senior firsthand Guide in Memphis, TN
What if it All Works Out? - My firsthand Journey
Introducing InquisitHealth: the proven power of peer-to-peer mentoring
Surreal, Beautiful and Bittersweet - From the Lyfebulb blog
Shirazian S, Grant CD, Aina O, Mattana J, Khorassani F, Ricardo AC. Depression in Chronic Kidney Disease and End-Stage Renal Disease: Similarities and Differences in Diagnosis, Epidemiology, and Management. Kidney Int Rep. 2016 Sep 20;2(1):94-107. doi: 10.1016/j.ekir.2016.09.005. PMID: 29318209; PMCID: PMC5720531.
Cutler RL, Fernandez-Llimos F, Frommer M, Benrimoj C, Garcia-Cardenas V. Economic impact of medication non-adherence by disease groups: a systematic review. BMJ Open. 2018 Jan 21;8(1):e016982. doi: 10.1136/bmjopen-2017-016982. PMID: 29358417; PMCID: PMC5780689.
![Signals From [Space]](https://substackcdn.com/image/fetch/w_80,h_80,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F55686857-6b99-45a6-ac0f-09c9f023f2a0_500x500.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/e_trim:10:white/e_trim:10:transparent/h_72,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F4d588ac1-7fac-4bd4-829d-fc7b4e8f1326_1512x288.png)

![Signals From [Space]](https://substackcdn.com/image/fetch/w_36,h_36,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F55686857-6b99-45a6-ac0f-09c9f023f2a0_500x500.png)