How should we deliver kidney care in rural America?
Lessons from the Zuni tribe and VA on home-based care and tele-nephrology
One in five Americans and about 86% of the land area in the United States are considered “rural.”1
In the vast landscape that is America, chronic diseases cast long shadows, affecting peoples’ lives in real, complex and inequitable ways. They are the leading causes of death and disability in this country; and yet, these battles are louder in some corners of the country than others. Providing quality healthcare for these 60 million people has its own set of uniquely rural challenges: a shortage of healthcare workers, limited access to specialists (like kidney doctors), and daunting distances to reach care. But that’s only the beginning of our unequal reality. When we consider race, ethnicity, and the growing diversity of rural America, it’s clear this may be one of the defining challenges of our time.23
Today, we continue our journey into the kidney space through the lens of rural healthcare. We begin with two stories of decades-long efforts to bridge nations.
IN THIS ISSUE
Lessons from the Zuni Indians on home-based kidney care
How tele-nephrology is extending kidney care to 5 million rural veterans
Why it matters and what’s next in this space
1. What Zuni Indians teach us about community-led, home-based kidney care



This first story is nearly 30 years in the making. In 1995, a Zuni governor needed a kidney transplant and sought care in Albuquerque. It was then that UNM researchers learned members of the Zuni tribe are 18.5 times more likely to develop kidney failure.4
Fast forward to 2013, when a team of researchers and Zunis co-designed a Home-based Kidney Care (HBKC) treatment program for adult Zuni Indians living with CKD in rural New Mexico (see images). The team employed community health representatives (CHRs) under physician supervision to deliver culturally tailored, state-of-the-art health care in the patient’s home environment.5
Here’s how it worked:
The program had (5) major interventions: (1) biweekly home visits; (2) tailored lifestyle coaching & education; (3) point-of-care (POC) lab testing; (4) daily motivational text messages for the first four months; and (5) telehealth services based on the Project ECHO model.
Trained Zuni CHRs were vital. They completed extensive training in lifestyle coaching, diabetes prevention, and diet and exercise change, which played a key role in delivering the interventions (daily texts, bi-weekly visits, lab tests, education) and support for participants.
The study involved extensive community outreach, including news outlets and education sessions in schools, senior and wellness centers, and other community events and locations. The research team also maintained regular meetings with CHRs, tribal leaders and advisory panel members who helped design the program.
Results: The HBKC program improved participants’ activation in their health and health care (primary outcome, measured by the PAM), and reduced markers of and risk factors for CKD (secondary outcomes, including BMI, A1c, and mental quality of life score).6
Milestones: The UNM research team is now expanding the initiative to screen 600 new participants from four additional New Mexico tribes.7
2. How tele-nephrology is extending kidney care to 5 million rural veterans
The Department of Veterans Affairs (VA) has a history of pioneering innovations in kidney care, from the AV fistula to the first national dialysis program. Today chronic kidney disease (CKD) is the fourth most common diagnosis across the VA. In response, the VA has implemented a tele-nephrology program that it deploys through its hub and spoke care model.8
Here’s why and what we’ve learned so far:
Problem: 5 million veterans live in rural areas. Despite the fact veterans have higher rates of kidney disease than the general US population, rural veterans struggle to access specialist nephrology care. Only 38% of veterans with CKD meet with a nephrologist prior to developing kidney failure.9 Maybe that helps explain why one in ten new dialysis patients each year in the US is a veteran.10
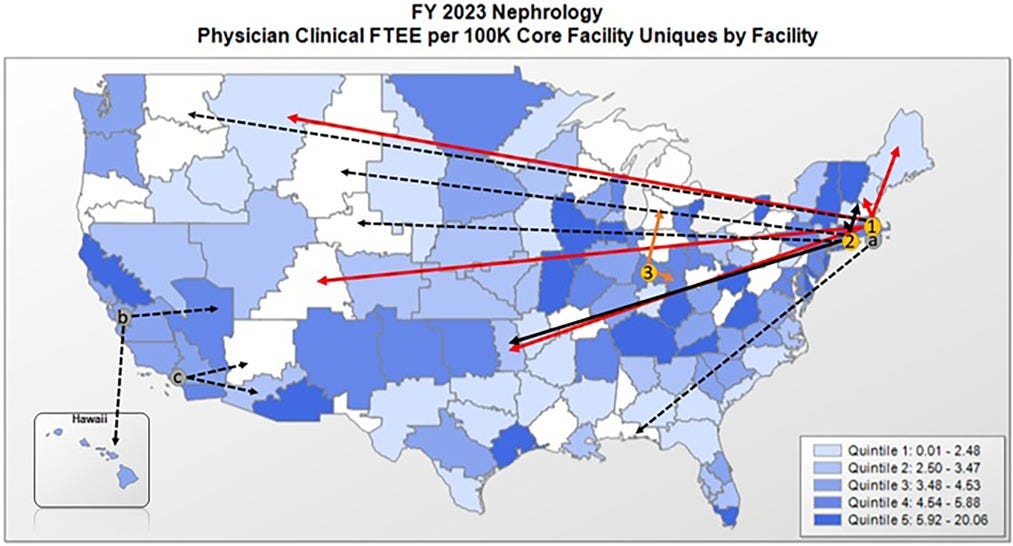
Solution: To address the need for rural nephrologists, a team of VA researchers developed a tele-nephrology program using a hub and spoke design to connect nephrologists located in hubs (Boston, Connecticut) with patients in spoke sites like Maine, New Hampshire, Colorado, and Montana.
RE-AIM Study: A 2023 study of that VA tele-nephrology program provides helpful insights on perceptions and experiences among (14) staff members and clinicians at (5) spoke sites. Here are 5 takeaways using the RE-AIM framework:
Reach: Active engagement of a centralized clinical champion was a key factor in early success of tele-nephrology program.
Effectiveness: Transition from community-based nephrology to VA tele-nephrology was heralded as the most meaningful indicator of the effectiveness of the intervention.
Adoption: Effective adoption strategies included bi-weekly training with Hub nephrology staff and engagement of nurse practitioners.
Implementation: Meeting the needs of Veterans through proper staffing during tele-nephrology examinations was a key priority in facility program implementation.
Maintenance: Growing reliance on Hub nephrologists may give rise to insufficient availability of nephrology appointments in some Spoke sites.
Milestones: A hub in Providence, RI opened in July and negotiations are currently underway to expand to west coast hubs in Palo Alto and Long Beach, CA in FY24 and FY25 (see image).
WHY IT MATTERS
Earlier this week I read an article by physician-journalist Kay Miller Temple that struck a chord (and inspired this piece). She cites a 2022 paper with several rural data points on kidney health worth considering:
Nearly 240,000 rural Americans have ESRD
Over 15,000 rural patients started dialysis in 2017, about 15% of all new dialysis starts nationwide for that year
Rural dialysis facilities were less likely to offer home dialysis as an option
Rural patients were more often on home dialysis, but only because they traveled to urban dialysis centers for care
No matter where patients received dialysis care — urban or rural — rural dialysis patients have a worse mortality rate, a concerning data point because it's not directly linked to dialysis facility location
One question that came to mind while reading these papers is how future dialysis policy can bridge the access gap for rural patients. American Kidney Fund President & CEO LaVarne Burton penned a piece on this exact topic earlier this year, calling on Congress to reintroduce the CARE For All Kidneys Act.11
What does a policy solution look like? Telehealth access, expanded reimbursement, public-private partnerships, regulatory reform, home dialysis support(s), community health worker programs? I’d love to hear from you.
WHAT’S NEXT
Last week I shared a LinkedIn post about this topic that started with a quote:
“Doc, I was told I have stage 5 kidney disease. What happened to stages 1 through 4?”
Dozens of comments came in. Thanks for sharing your thoughts and experiences, and please keep doing so. I wanted to share a few of them with you here:
Kimberlee Langford: “Boy! If I had a nickel for every time I have heard that!”
Karla Rippchen: “This post spoke to my heart. I grew up on a rural ND farm and currently live in Iowa. Three small dialysis clinics closed their doors in the past two years in my area requiring the caregivers of some of these patients to drive 60+ miles one way to a dialysis center as they were not home dialysis candidates.”
Matt Weeks: “The tragedy is exactly that: what happened to “stage-1-4” and what is happening, systemically, that keeps it somehow hidden and/or unaddressed.”
Alex Berrios: “My time at the University of Kentucky traveling to the dialysis centers all over the rural areas of my state. It saddens me that patients didn’t have the resources to be successful with their care. To either not get their options given to them…or at times they don’t want to be bothered and just stay on “the dialysis “. How do we make that change? How do providers do it?”
Conclusion
Kidney care is a massive, growing piece of the healthcare pie. But for 60 million people in 86% of the land, it’s not just out of mind— it’s out of reach.
As we continue our journey into the kidney [space], we must remember that, in the vast landscape of America, the battle against chronic diseases like CKD remain a defining challenge. Keep exploring, and keep fighting.
The Signals newsletter is supported by healthtech explorers like you. Thanks for your support and keep exploring, my friends.
Ibid.

![Signals From [Space]](https://substackcdn.com/image/fetch/e_trim:10:white/e_trim:10:transparent/h_72,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F2efc1ef1-ba0b-4ca3-b9f6-a9a790da4b38_1344x256.png)

![Signals From [Space]](https://substackcdn.com/image/fetch/w_36,h_36,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2Fa4736f49-6a20-4fd6-a3de-d48cb4b105f2_375x375.png)