Signals Recap: Azar on VBC, Carilion-UVa, TransMedics, JPM Takeaways, Ozempic, Vafseo, & More...
A collection of news, research, funding & community voices shaping the future of global kidney health
Welcome back, we’ve missed you. This is our first update of 2025, and it’s a fun one. A new year means new funding, new research, new jobs, and even a new look for us here at Signals HQ. There are two changes you can expect from our recaps going forward: they’ll be more consistent (Sundays, not anydays), and they’ll be more to the point (five or ten minutes, not fifty).
To support these changes, we’re tidying up our format. We’ll focus on the 2-3 stories you should know about and why they matter, followed by curated lists of headlines, research, community updates and open roles across the Kidneyverse.
As always, I’d love to hear from you. Leave a comment or join us in Signals Slack to let me know what you think of the new format, cadence, and branding. Let’s light this candle, shall we?
In this issue
Alex Azar and “pulling the band-aid” on VBC
Carilion makes its case for kidney transplant
Fraud allegations against TransMedics
How CMS builds evidence-based care models
Why dietitians should take charge of renal nutrition
A petition for patients to know about organ offers
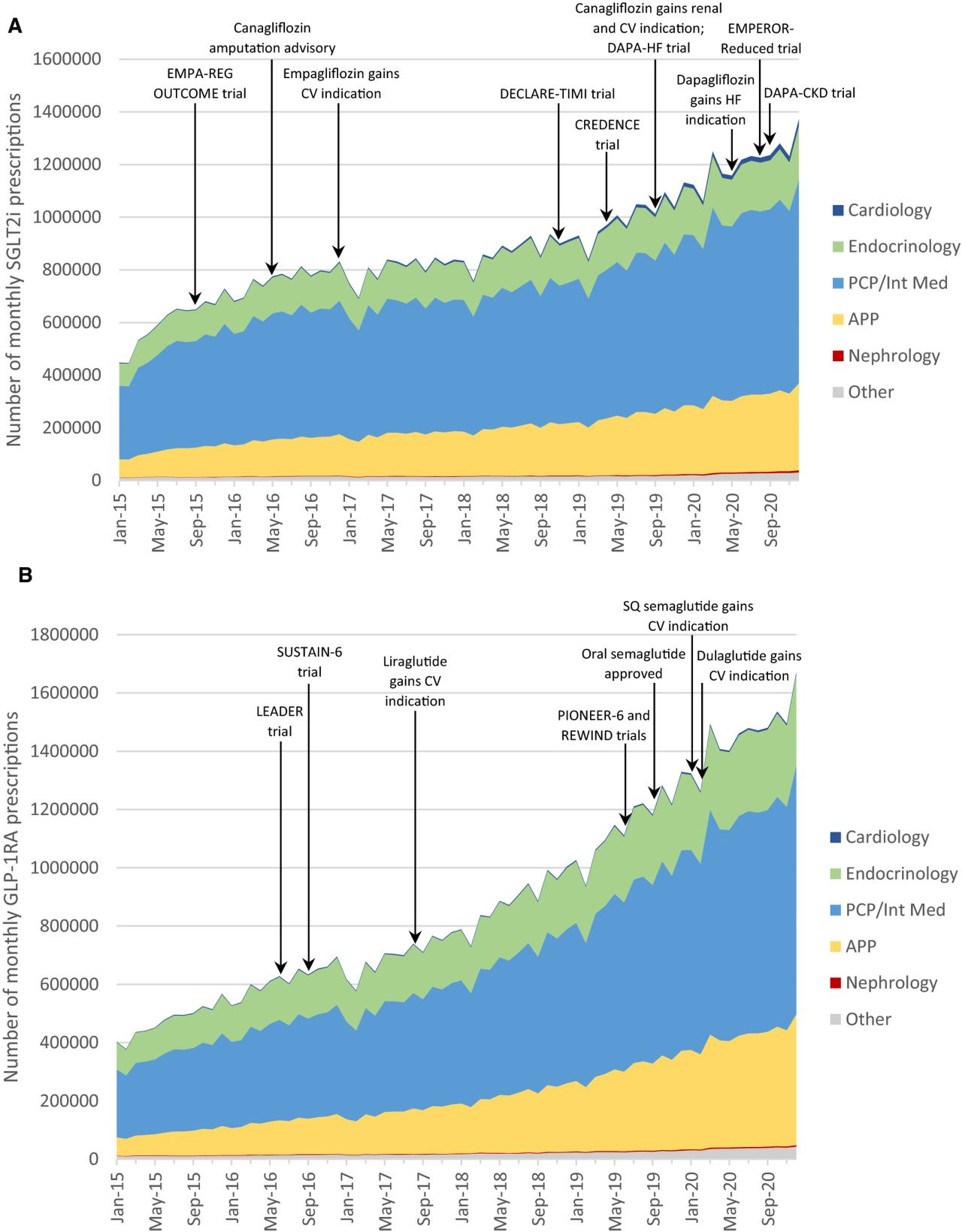
SGLT2 prescription patterns by specialty (2015-20)
Studying the gut-kidney-PKD axis in Cameroon
Open roles around the Kidneyverse
& more…
Updates
ICYMI: We just re-launched our data room with new resources and formats (PDF, PNG, XLSX), and made it a bit easier to navigate. Going forward, you’ll be able to find all our visuals, one-pagers, and databases there. We also added the direct link in our navigation bar on the Signals homepage so it’s easy to find when you need it.
Good news: we’re also opening up the Slack #general channel so you can join the conversation and see the magic firsthand. I’m loving the back and forth questions, discussions, and candor you just can’t get on social media. People helping people. Paid subscribers get full access to all channels like #transplant, #dialysis, #VBC, #policy, #jobs, #questions and more.
Signals
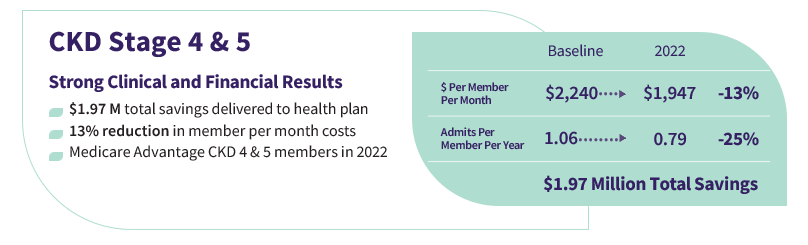
“Time to Rip the Band-Aid Off”: Alex Azar on Value-Based Care's Future
Summary: At the 2024 Fierce Health Payer Summit, former HHS Secretary Alex Azar urged the healthcare industry to fully commit to value-based care, citing progress in kidney care models as a foundation for broader reform. He highlighted data showing improved patient outcomes and cost savings from government and commercial kidney value-based programs, including increases in home dialysis, depression screening, and transplant waitlisting. Azar argued that kidney care's holistic approach makes it an ideal testing ground for pay-for-performance models and called for large-scale adoption across the healthcare system. Despite progress, Azar noted persistent challenges, including aligning incentives, improving clinician buy-in, and addressing gaps in data sharing and interoperability. He stressed the need for reliable government support and better data tools, such as predictive analytics for identifying high-risk patients. Looking ahead to 2025, Azar remains optimistic, emphasizing that the time has come for the healthcare system to stop experimenting and fully embrace value-based payment models to achieve transformative change.
Thoughts: Three calls to action here: align incentives, improve clinician buy-in, and enhance data sharing. The first two make sense to me: they take time and move at the speed of trust. The third I still struggle with as far as whether access to “good” data is a limitation of policy or technology. The latter seems unlikely. Either way, I think a bit more accountability and transparency in VBC performance (and stable goalposts) would be a great thing. And it’s “good” timing for a spark, given the recent blog from CMMI and kidney-friendly leadership changes headed to Washington this week. When I think about alternative payment models, particularly a second-gen model like Kidney Care Choices (KCC), I think about reach. My last (unofficial) count is in the ballpark of 1 million lives served across 11 providers, but I’ll be sharing that full breakdown here soon enough.
What do you think it will take to get to a full embrace of VBC? What would that even look like? For patients? For providers? For policy makers?
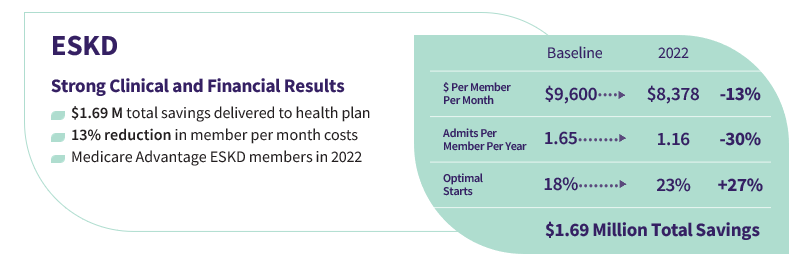
Carilion makes its case for opening Roanoke Kidney Transplant Center

Summary: Carilion Clinic is advocating for the establishment of a kidney transplant center at Roanoke Memorial Hospital to serve Southwest Virginia's 40,000 chronic kidney disease patients. Currently, patients like Joey Shervey, diagnosed with stage 5 renal failure, face long trips to Charlottesville’s UVA Hospital for care. These burdens, both physical and emotional, highlight the need for localized care. Despite strong community support—including hundreds of letters and patient testimonies—the proposal faces opposition from UVA, concerned about its impact on their program. Carilion argues that a local transplant center would improve accessibility, reduce risks, and provide better outcomes for patients. The state health commissioner will review Carilion’s proposal and issue a decision in the spring.
Thoughts: This conversation ultimately comes down to balancing accessibility with quality care. Miriam Godwin reminded me of an important adage: once it's been granted, every healthcare entity will defend its market. Naturally, this complicates the entry of newer, smaller players. Ann Kempski pointed out that transplant centers of excellence are crucial, but the Certificate of Need (CON) process often fails to consider rural areas like East Tennessee and West Virginia, where Carilion could address unmet needs. Alice Wei and Cosme also emphasized that bigger isn’t always better—larger centers may have better outcomes, but consolidation can harm patients, especially when smaller hospitals could provide essential care with the right resources. Liise Kayler highlighted the importance of proximity in rural areas, where logistical and social challenges often outweigh the benefits of larger institutions. The debate is about ensuring specialized care is accessible to everyone, no matter their location.
What do you think—is there such thing as too much competition when it comes to kidney transplant?
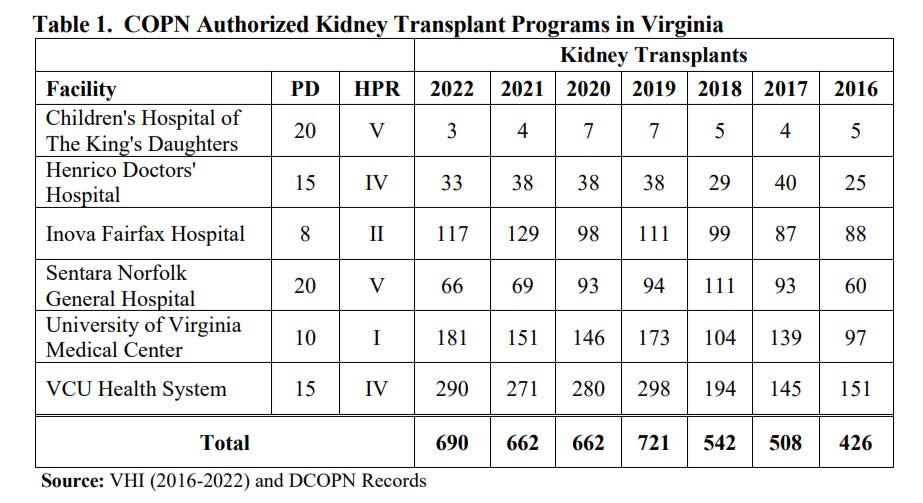
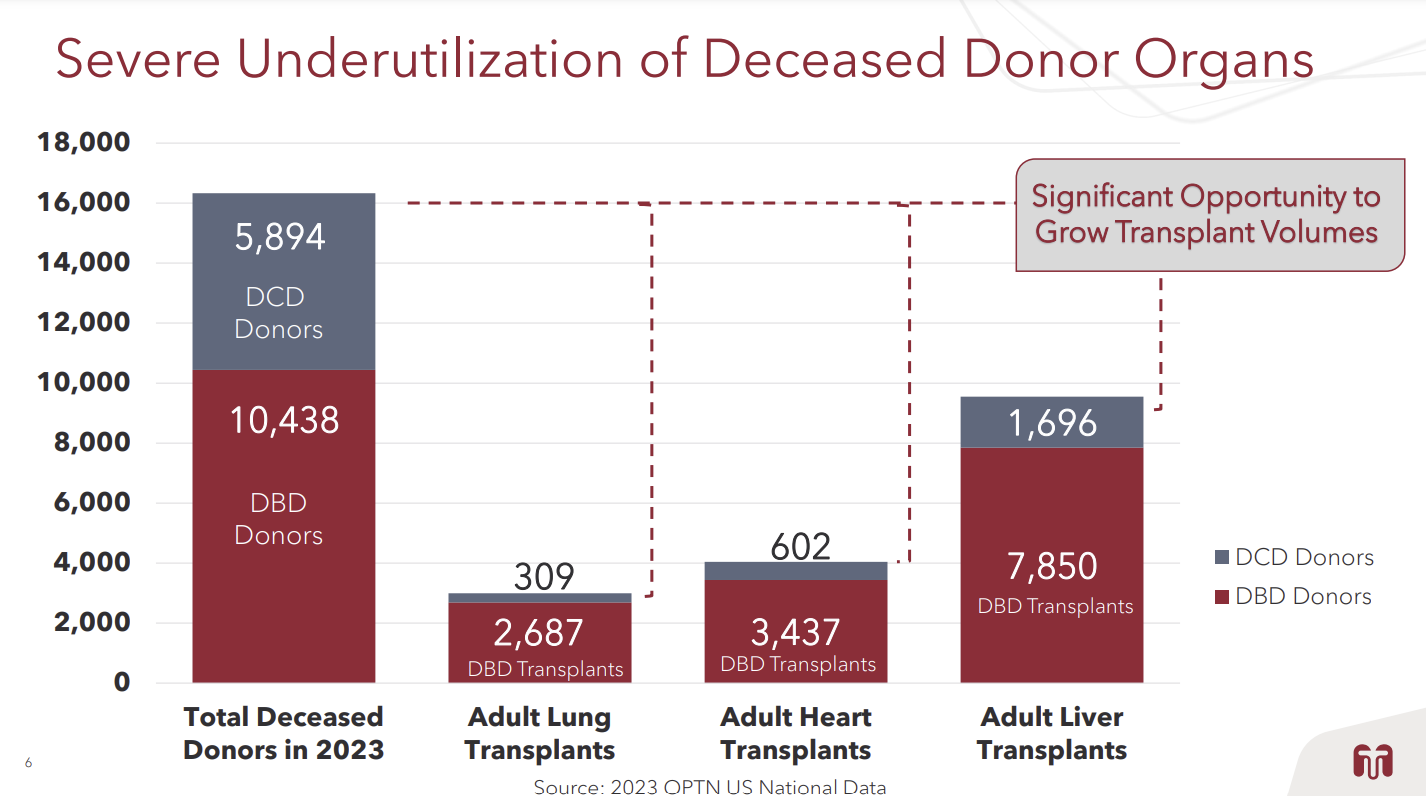
TransMedics Faces Allegations of Fraud, Organ Trafficking, and Ethical Violations
Summary: TransMedics is under scrutiny following allegations of fraud, organ trafficking, and unethical practices detailed in a report by Scorpion Capital. The claims, which include accusations of coercive business tactics, off-label use of its Organ Care System (OCS), and fraudulent billing, have triggered investigations by two shareholder rights law firms. In response, TransMedics has strongly denied the accusations, calling them baseless and aimed at market manipulation. Despite the controversy, the company remains focused on growth, including the launch of next-generation OCS programs in 2025, and highlights its role in enabling over 7,000 transplants with its technology. Shareholder investigations into potential securities law violations are ongoing.
Thoughts: The allegations against TransMedics raise serious concerns about ethics and oversight in organ transplantation. The 342-page Scorpion Capital report, based on six months of investigation and over 30 interviews, outlines key accusations against the company. While TransMedics firmly denies the claims, the ongoing shareholder investigations highlight the risks for patients and investors alike. As TransMedics looks to expand its Organ Care System (OCS) into heart and lung programs, this analysis offers a solid breakdown of the report’s main allegations, plus possible outcomes (not an issue, bad news, worst case).
What should we know about this space that we may not? Where do these types of technologies intersect with policy and broader calls for system reform?
Visual of the Week
We often hear primary care and cardiology play a major role in managing kidney disease early. It's worth noting most prescriptions for both SGLT2is and GLP‐1s are provided by PCPs/internists. In 2020, this group accounted for the majority of national SGLT2i (57%) and GLP‐1 (52%) prescriptions, followed by advanced practice providers (24% and 26%), endocrinologists (15% and 19%), cardiologists (1.5% and 0.4%), and nephrologists (0.5% and 0.3%). That tiny sliver of red at the bottom of each chart is nephrology. The first approval for treating CKD arrived in April, 2021— what do you think the chart looks like now? See full comment thread here.
News
Novo’s Ozempic, Wegovy Targeted in Second Round of IRA Drug Price Negotiations [BioSpace]
At JPM, biotech industry expresses excitement — and some anxiety — about therapies from China [STAT]
With a major patent cliff coming, will JPM play host to some serious deal-making? [STAT]
Maze Therapeutics looks for IPO lodestar to guide kidney disease assets through clinical trials [FierceBiotech][S-1]
Metsera files IPO just 9 months after emerging [FierceBio][S-1]; also announces positive results in newest Phase IIa GLP-1RA [Clinical Trials Arena]
Trump administration will likely kill the FTC’s controversial noncompete rule [Healio]
Patient care technicians are key in dialysis but are often not fairly recognized [Healio] (H/t Paul Gordon)
Research
Lived Experiences of Patients Hospitalized With Acute Decompensated Heart Failure and Kidney Dysfunction [JAMA]
The survival of B cells is compromised in kidney disease [Nature]
Vafseo trial update: more than 750 patients have now been enrolled in the VOICE study [U.S. Renal]
Immunogenomic determinants of exceptional response to immune checkpoint inhibition in renal cell carcinoma [Nature Cancer]
Gut microbiota and kidney function in autosomal dominant polycystic kidney disease participants in Cameroon: a cross-sectional study [BMC Nephrology]
Belzutifan plus cabozantinib as first-line treatment for patients with advanced clear-cell renal cell carcinoma (LITESPARK-003): an open-label, single-arm, phase 2 study [Lancet]
Community
Policy: Successor Models, Scaling Pathways, and the CMS Innovation Center [CMS Blog] (H/t Miriam Godwin)
Petition: Patients Deserve To Know (about organ offers)! [NKF]
Industry: #FutureFresenius Presentation at JPM [Fresenius]
Industry: The 34 Lives team presented The First Dedicated Normothermic Rescue Center for Unused Renal Grafts [LinkedIn]
Perspective: Dietitians should take the lead in weight management for patients with kidney disease [Healio]
Public: New undergraduate organization provides free kidney disease screenings [Virginia Tech]
Jobs
Transplant - Hepatology at Piedmont Transplant Institute
Director, Product Strategy Lead - Renal at Novartis
Director of Product and Strategy at Monogram Health
VP, Business Development at Breakthrough T1D
Account Executive, Healthcare at Stepful
Senior Program Manager at Diality
Made Possible By
Signals is made possible with the generous support of our sponsors. We are grateful to partner with organizations committed to advancing kidney care and innovation. This post was made possible by Roivios and 3ive Labs. Thanks team!
![Signals From [Space]](https://substackcdn.com/image/fetch/w_80,h_80,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F55686857-6b99-45a6-ac0f-09c9f023f2a0_500x500.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/e_trim:10:white/e_trim:10:transparent/h_72,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F4d588ac1-7fac-4bd4-829d-fc7b4e8f1326_1512x288.png)

![Signals From [Space]](https://substackcdn.com/image/fetch/w_36,h_36,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F55686857-6b99-45a6-ac0f-09c9f023f2a0_500x500.png)




🚨 The Truth About Value-Based Care: A System Designed for Profits, Not Patients 🚨
Alex Azar’s relentless push for Value-Based Care (VBC) is not only misguided—it’s outright dangerous. His speech at the 2024 Fierce Health Payer Summit was filled with buzzwords like "aligning incentives" and "data sharing," but not once did he mention how VBC actually benefits patients. Why? Because it doesn’t.
Interwell Health, one of the biggest care coordination companies, is aggressively lobbying for VBC because it profits from controlling access to care—not from improving patient outcomes. Their real goal is aligning nephrologists and insurers to ration treatments, delay transplants, and maximize cost savings—all while pretending this is about “value.”
💰 The Real Purpose of VBC: Limiting Patient Access
VBC was supposed to revolutionize kidney care. Instead, it has:
Increased administrative burdens on nephrologists, forcing them to justify every decision to middlemen who have never treated a single dialysis patient.
Created more barriers to transplant referrals, because transplants cost insurers more in the short term—even though they save money and lives in the long run.
Pushed home dialysis as a cost-saving measure, not because it’s always best for the patient, but because it’s cheaper for the system.
Allowed private equity-backed coordination companies like Interwell Health to act as gatekeepers, deciding which treatments are “worth” the expense.
🚨 The Criminal Negligence of Alex Azar
Alex Azar’s speech reads like a sales pitch for insurers and corporate medicine, not an actual plan to improve care. He claims VBC is ready for full-scale adoption despite its failures in kidney care. But here’s what Azar conveniently ignores:
Where is the actual patient outcome data? "Increases in home dialysis, depression screening, and waitlisting" mean nothing if patients are still struggling to get transplants and still dying at alarmingly high rates.
Why does he downplay the rationing of care? VBC has created an incentive to deny life-saving treatments, yet Azar frames it as “cost savings.”
Why are insurers and corporate middlemen in charge of patient care? Interwell Health’s entire business model is to profit off denying or delaying access to care—not to improve patient health.
Azar’s push to force VBC into every corner of healthcare is a calculated move to enrich insurers, not protect patients. The fact that he cites kidney care as the model for VBC is terrifying—because kidney patients remain among the most vulnerable, underserved, and exploited populations in U.S. healthcare.
🛑 Patients Are Not Cost Centers. We Are Human Beings.
Value-Based Care is not about value—it’s about maximizing corporate profits by rationing care. If VBC truly worked, we would see better transplant rates, lower mortality, and fewer bureaucratic hurdles—not more corporate interference in patient decisions.
🔴 We need patient-first reform, not more cost-cutting schemes disguised as "value."
🔴 We need transparency in how these programs work—not another black box controlled by insurers and for-profit middlemen.
🔴 We need to dismantle the role of private equity in kidney care—before even more patients die waiting for care they should have received sooner.
Alex Azar, Interwell Health, and every other corporate lobbyist pushing this predatory model of care should be held accountable. The true cost of their greed isn’t just dollars—it’s the lives of kidney patients sacrificed for their bottom line.