Across the Kidneyverse: July, 2024
Living kidney donation, telemedicine trends, 2024 startup funding, and more!
Welcome back to Across the Kidneyverse, our monthly exploration of headlines, market movers, research and commentary from the past four weeks. This month, we hosted our first Signals Live audio event to give you a chance to meet your fellow explorers on the frontlines of kidney care innovation. Moving forward, we’ll use this forum to talk about the latest, greatest, and most pressing things happening in the kidney space. At the end of the day, this Signals is about bringing people together, celebrating our wins, hearing fresh perspectives, and creating space for productive, forward-thinking discussions in the kidney community.
Have tips or feedback? Hit reply or join the conversation here.
Reading time: 35 minutes
In this issue
Reminders
We’re all about experiments. This month we tried something new with our very first Signals LIVE audio event. If you’re one of the nearly 80 people who joined us earlier this morning, thank you for being part of something special. I didn’t know what to expect for our first one, but I left feeling giddy and incredibly optimistic about this new format. Follow me to stay tuned for the next one in August.
Kidneyverse Careers is the only place dedicated to bringing top talent + companies together across kidney care. We started sharing a few open roles per month in each issue of this newsletter. Reach out if you want to highlight your company’s roles!📣
The Signals Inbox is always open to anyone who wants to share news, tips, and updates that belong in this monthly recap. It’s anonymous, so let me know what you’re seeing and hearing out there that people should know about!
Headlines
Here’s what caught my eye across the Kidneyverse this month, organized by topic.
Discovery & Innovation
Covering the latest in research, development, and clinical breakthroughs.
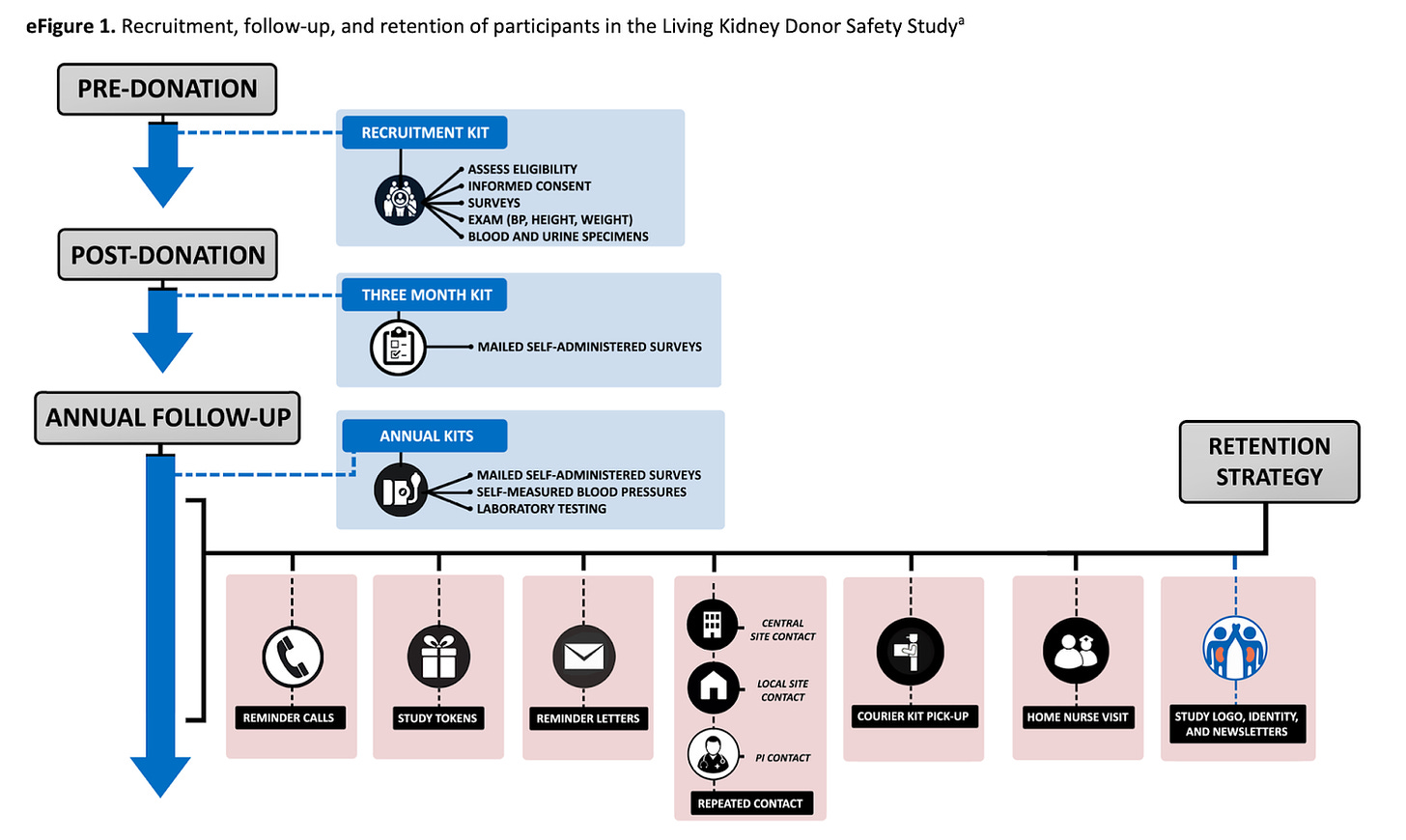
NephJC highlighted a recent study by Garg et al. that investigated whether living kidney donors face increased risks of hypertension and adverse kidney outcomes compared to non-donors. Living donor kidney transplants, which make up about 39% of total kidney transplants annually, show better survival rates than those from deceased donors. However, the long-term health risks for donors remain unclear. This study aims to provide clearer insights and improve counseling for potential donors, addressing the current gap in high-quality, long-term research on donor health outcomes. (JAMA)
Surgeons at Northwestern Medicine Comprehensive Transplant Center successfully performed their first kidney transplant on an awake patient, a technique that could benefit those with severe heart or lung issues who are at high risk for general anesthesia. Strive Health's Chief Nephrologist, Amit Kapoor, recently shared his thoughts with MDLinx on how this approach could lead to safer surgeries for high-risk kidney transplant candidates, potentially expanding access to life-saving transplants for patients previously deemed too risky for traditional methods.
In Blacksburg, VA, a unique research farm is raising piglets under stringent biosecurity measures to grow kidneys and hearts for human transplants. These gene-edited pigs, developed by Revivicor Inc., live in an environment cleaner than that required for humans, with filtered air, disinfected feed, and strict hygiene protocols. The facility, designed to meet FDA standards for xenotransplantation, represents a $75 million investment. Pigs enjoy luxury conditions, including music and toys, highlighting their value and intelligence. A new 77,000-square-foot pathogen-free facility in Christiansburg signals a new phase, aiming to produce 125 pig organs annually for clinical trials, with plans for even larger facilities if successful—United Therapeutics could produce up to 2,000 organs a year in several places around the country. (H/t Paul Gordon for sharing)
Renalytix announced it has partnered with the innovative Steno Diabetes Center Copenhagen to enhance awareness and access to precision medicine for type 2 diabetes and early-stage chronic kidney disease patients. This collaboration marks the first use of Renalytix's KidneyIntelX technology outside the U.S., highlighting its clinical utility in the European Union. The AI-enabled, biomarker-based blood test aims to improve early prognosis of CKD progression in type 2 diabetes patients, fostering precision-based care globally. This news comes after KidneyIntelX received FDA approval, inclusion in KDIGO clinical guidelines, and full Medicare coverage. (Press release)
DeLorean AI, in partnership with Innovative Renal Care (IRC), has released a white paper titled "Transforming Renal Care: Improving Patient Care by Leveraging AI Insights." This paper details the impact of DeLorean AI’s Medical AI solution, which, during a 3-month pilot in 17 IRC dialysis centers, resulted in a 27% decrease in hospitalizations due to fluid overload. The AI solution predicts missed treatments, hospitalizations, and other key measures like adequate clearance and anemia management. Integrating AI into daily workflows has improved patient outcomes, treatment adherence, and resource allocation, demonstrating significant benefits for renal care. (H/t Sev for sharing)
In the latest episode of BackTable Innovation, Dr. Sabeen Dhand interviews Dr. Ali Golshan, an Interventional Radiologist in Los Angeles, about the complexities of managing superficial venous disease. Dr. Golshan discusses the latest advancements in thermal and non-thermal ablation techniques and introduces his innovative medical device, SOLVEIN™, designed to improve treatment outcomes. The episode also offers practical tips for managing venous insufficiencies and insights into the entrepreneurial journey of developing a new medical device. (Listen on Spotify)
Spencer Dorn and François Chollet highlight the limitations of Large Language Models (LLMs) in clinical settings, emphasizing that LLMs, which rely on memorization and pattern matching, lack the adaptability needed for complex medical tasks. In a discussion about the $1 million ARC-AGI Prize, François Chollet explains that the ARC benchmark challenges LLMs with novel puzzles requiring core knowledge, underscoring their insufficiency for achieving Artificial General Intelligence (AGI). For clinical applications, Dorn and Chollet advocate for hybrid AI systems that combine LLMs with other approaches to enhance reliability and effectiveness in patient care.
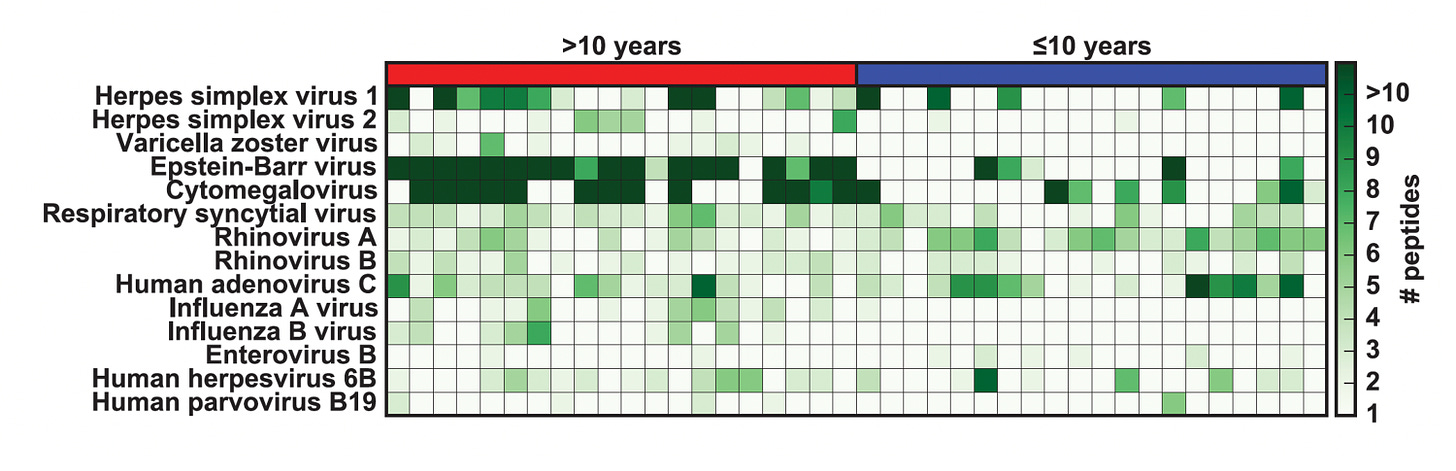
In his recent article for Ground Truths, Dr. Eric Topol emphasizes the need for an "immunome" to measure the immune system's health more precisely. Despite the critical role of the immune system in fighting infections, diseases like cancer, and indicating aging, there is no comprehensive clinical test to evaluate it. Current methods, like the neutrophil-to-lymphocyte ratio (NLR) from a complete blood count (CBC), are crude and not individually informative. Dr. Topol highlights the potential of advanced technologies like VIrScan, which can detect antibodies to over 1,000 virus strains from a single blood drop, to revolutionize immune health assessment.
Market Insight
Trends, funding updates, industry developments & analysis.
Cigna is expanding its partnership with Interwell Health for its value-based care offerings for patients on dialysis. Interwell and Cigna began have worked together since 2017 to support dialysis patients being treated at Fresenius clinics. This new expanded program will now include patients not previously covered under value-based care contracts. According to the release, Interwell’s program will coordinate appointments and transportation, provide coaching, and implement a risk-stratification process to reduce hospitalizations and improve patient outcomes.
Cigna also announced it is expanding its Healthmap Solutions CKD Program to 27 additional markets starting in August. Healthmap’s program focuses on pre-dialysis disease management for vulnerable patients, and is currently available in Florida, Georgia, North Carolina, and South Carolina. The initiative aims to improve clinical outcomes, reduce ER visits and hospital admissions, identify care gaps, and provide monthly patient-specific recommendations.
Baxter is in exclusive talks to sell its kidney care business, Vantive, to private equity firm Carlyle Group for over $4 billion, according to The Wall Street Journal. Talks began in late June, and a deal could be announced soon, though it's not finalized. Initially, Baxter planned to spin off Vantive into a separate publicly traded company but later considered selling the segment to private equity. Baxter has not commented on these market rumors — it sounds like Carlyle has lined up $3 billion in debt to finance the transaction.
Chris Turitzin's latest report in Single Aim reveals key trends in the telemedicine industry by analyzing the work history of 115,000 clinicians. Telemedicine is particularly thriving in mental health, employing over half of all telemedicine clinicians. However, other telemedicine sectors are still recovering from inflated expectations and over-funding. Despite high demand for remote clinical jobs, telemedicine companies remain a small niche, representing just 3-4% of medical clinician jobs. This highlights both the potential and the challenges within the industry.
Adona Medical, part of the Shifamed portfolio, has secured $33.5 million in Series C financing to advance the development and clinical trials of its novel interatrial shunt and remote monitoring solution for heart failure patients. The innovative device, featuring an adjustable shunt and integrated sensors for continuous pressure monitoring, aims to offer a more individualized treatment approach. This funding will support the next stage of product development and early clinical experiences, aiming to address limitations of first-generation heart failure devices. The technology promises to enhance patient care by providing detailed hemodynamic data, allowing for better-informed medical management.
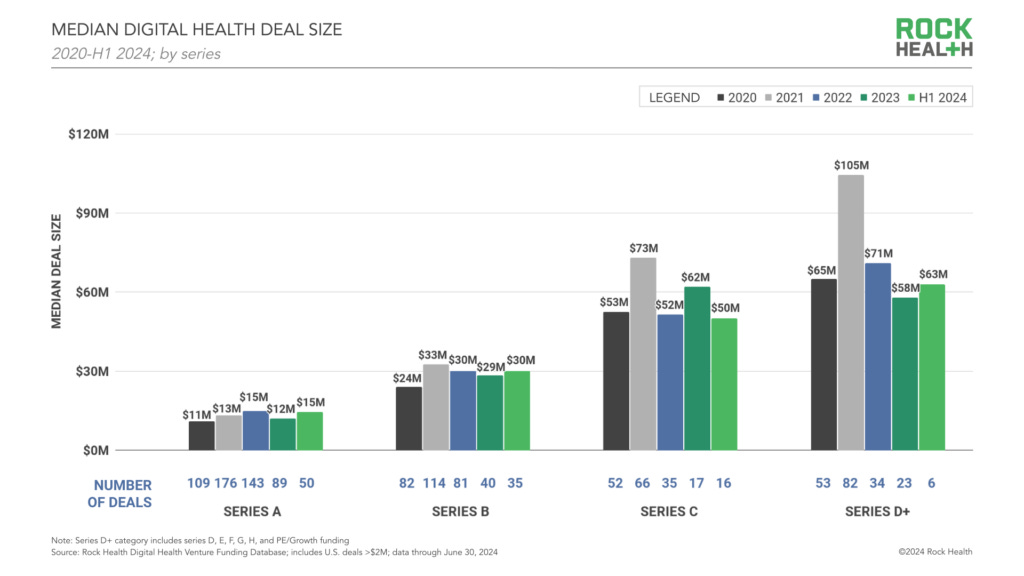
Rock Health reports that digital health startups raised $5.7 billion across 266 deals in the first half of 2024, suggesting the year could surpass 2023 if the investment pace continues. Key trends identified by Rock Health Advisory's Adriana Krasniansky, Mihir Somaiya, and Sari Kaganoff include early-stage deals making up 84% of labeled raises, a decline in unlabeled fundraises, AI-driven startups securing 34% of total sector funding, and early signs of revival in the digital health IPO market.
Digital Health New York (DHNY) released its H1 2024 New York Healthcare Innovation Report, revealing a significant increase in funding. Fifty-six companies raised $2.2 billion in the first half of 2024, a 35% increase compared to the same period last year. This surge in funding highlights the positive momentum within the NY digital health community as it heads into the second half of the year. DHNY Co-Founder and CEO Bunny Ellerin shared the latest report, emphasizing the growing enthusiasm and investment in healthcare innovation.
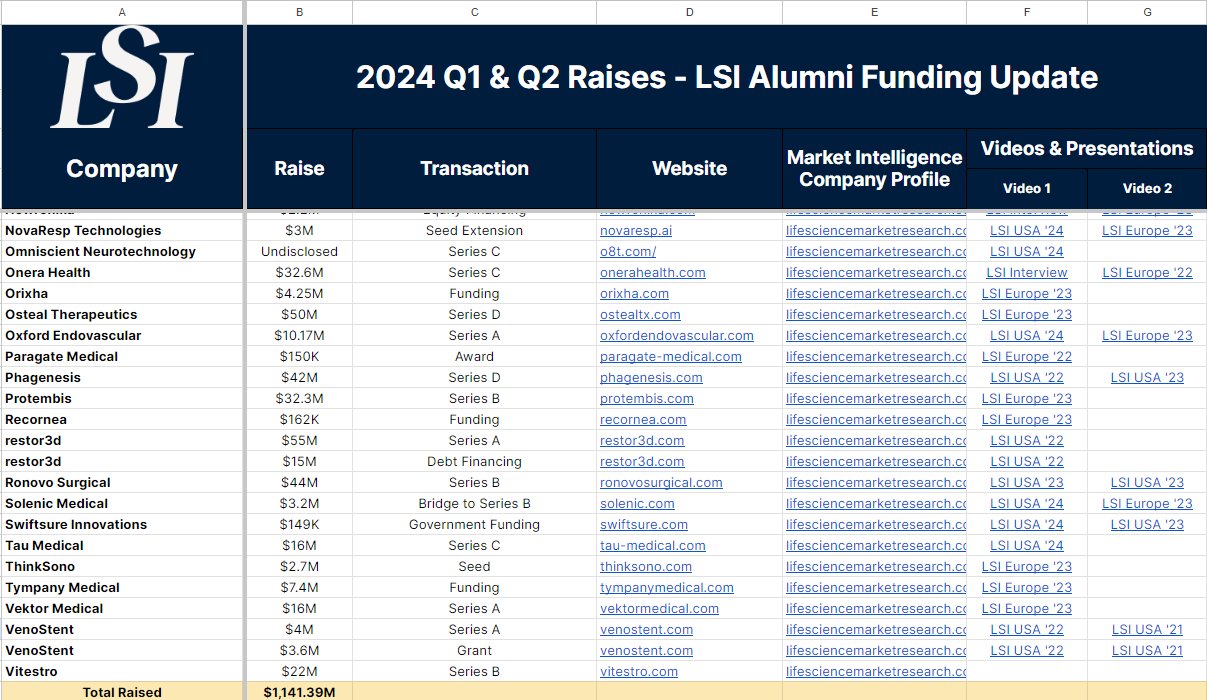
LSI has released its Q1 & Q2 2024 LSI Alumni report, showcasing the medtech and healthtech startups that secured funding in the first half of 2024. This report highlights the ongoing support and advocacy for innovation in the med device and life sciences sectors provided by LSI through impactful meetings and market intelligence. The report includes detailed information on the companies, funding amounts, transaction types, video presentations, and the lead and follow-on investors involved.
In a challenging market, private biotechs are increasingly pursuing both IPOs and buyouts simultaneously, as detailed by Endpoints News. This dual strategy allows companies to remain flexible amid a slight uptick in public debuts and a surge in biopharma M&A activity. Jonathan Norris of HSBC highlights that most biopharma companies consider both M&A and IPO opportunities. With biopharma M&A on the rise since early 2023, private biotechs are becoming attractive targets for larger pharma companies seeking to offset revenue losses from expiring patents. The median upfront deal size for private buyouts reached $1 billion in the first half of 2024, significantly higher than the annual average of the past six years.
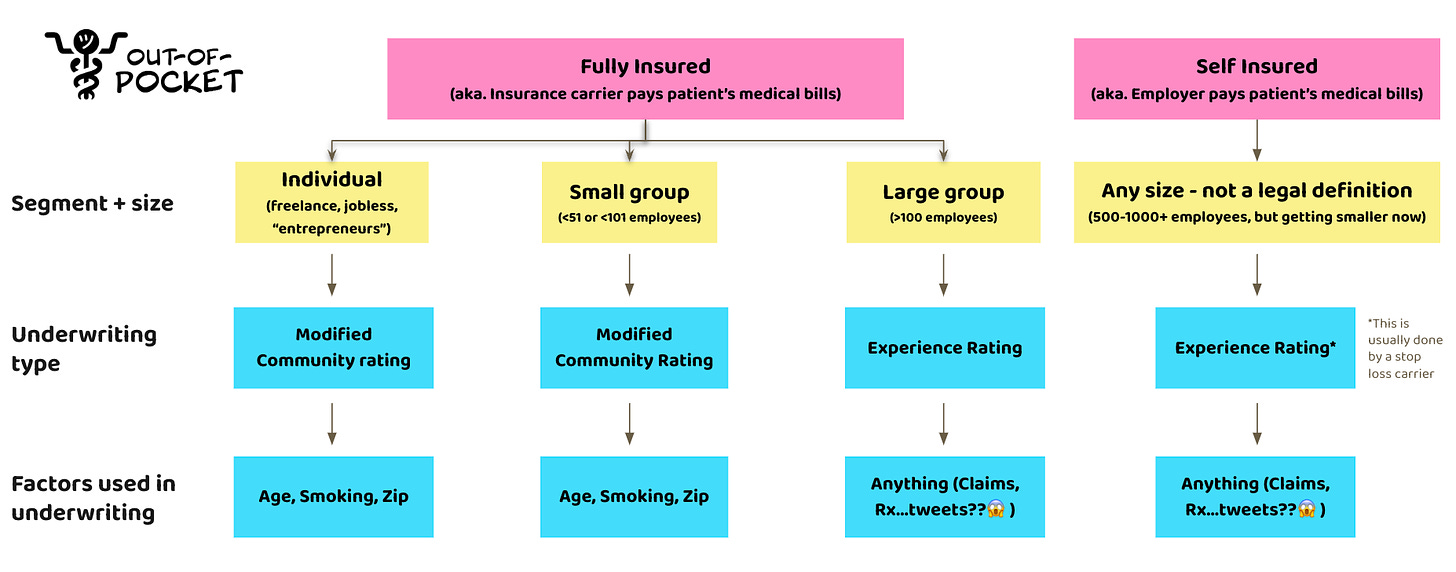
In his latest Out of Pocket newsletter, Nikhil Krishnan dives into the nitty-gritty of small group health insurance for small businesses—a tricky and often messy part of the market. Small businesses usually go for fully insured plans, where they pay premiums to health insurers who then cover any big medical bills. This "small group" market includes companies with fewer than 50 employees (or 100 in some states), covering about 8.5-9 million people, including dependents. He breaks down how underwriting works, shedding light on why offering affordable health insurance is so challenging for small businesses and why it's crucial for reducing labor costs and helping small businesses thrive in the U.S.
Policy & Regulation
Updates on policies, regulations, and government initiatives.
The Federal Trade Commission (FTC) has launched an antitrust investigation into major dialysis providers Fresenius and DaVita. According to Politico, the probe is examining whether these companies are engaging in anti-competitive practices by restricting physician mobility and limiting patient treatment options, including home dialysis. Learn more about the probe and non-compete agreements in my latest Signals Brief.
The American Association of Kidney Patients (AAKP) has joined a lawsuit against the Centers for Medicare and Medicaid Services (CMS), challenging the inclusion of oral-only phosphate-lowering therapies (PLTs) in the CMS End-Stage Renal Disease (ESRD) Prospective Payment System (PPS). The lawsuit, in collaboration with the National Minority Quality Forum (NMQF) and Ardelyx, argues that current phosphorus management therapies are burdensome and ineffective for many kidney patients. Despite the FDA approving a new, less burdensome oral therapy in 2023, CMS's decision is seen as federal overreach, potentially compromising patient care. Effective phosphorus management is crucial for dialysis patients to prevent severe complications and reduce mortality risks.
Town Hall Ventures’ Andy Slavitt and Andie Steinberg recently shared their perspectives on the Centers for Medicare & Medicaid Services' (CMS) CY 2025 Medicare Physician Fee Schedule proposed rule, which represents a significant shift toward integrating value-based care within a fee-for-service framework. They believe this proposal aims to make value-based care priorities more accessible, providing payment opportunities without the usual risks and regulatory challenges.
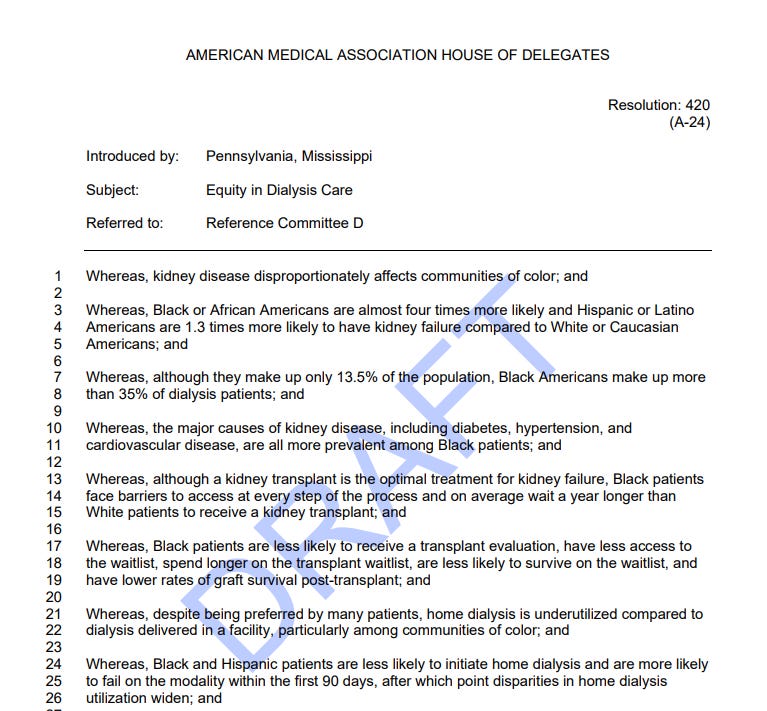
The American Medical Association (AMA) has introduced the Equity in Dialysis initiative to address significant disparities in kidney disease and dialysis care affecting communities of color. Black and Hispanic patients face higher rates of kidney failure and encounter numerous barriers to optimal treatment, including longer wait times for transplants and underutilization of home dialysis. The initiative aims to increase equitable access to all dialysis modalities by identifying and implementing economic, cultural, clinical, and technological solutions. The AMA emphasizes the importance of collaborative efforts to improve outcomes and reduce disparities in kidney care. (H/t Tom Mueller for sharing)
Congress is revisiting efforts to mandate quicker reviews of treatment requests by Medicare insurers, addressing a practice widely criticized by patients and doctors. The bipartisan bill aims to enshrine recent Biden administration reforms on prior authorization into law, protecting against future rollbacks and potential Supreme Court decisions that could limit federal rulemaking. Insurers use prior authorization to curb unnecessary care, but it creates significant administrative burdens for doctors and delays necessary treatments for patients, contributing to professional burnout and potentially impacting patient outcomes. Here’s what Humana President / CEO Jim Rechtin had to say about it on LinkedIn. (Axios)
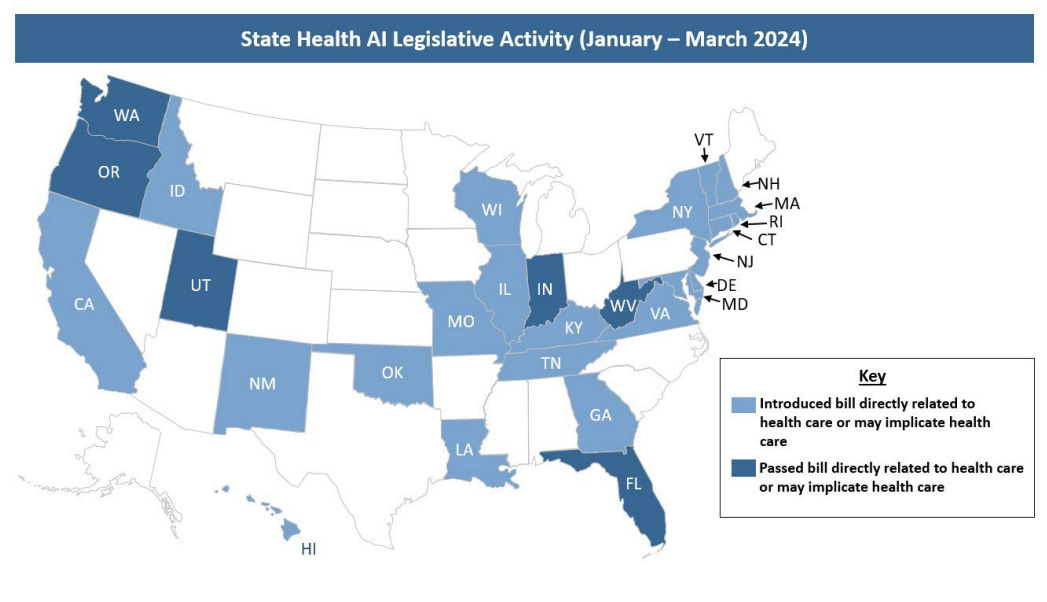
Christina Farr and Randi Seigel's article in Second Opinion outlines how U.S. policymakers are regulating AI in healthcare, aiming to balance its promises while preventing potential harm. The American Hospital Association (AHA) suggests AI regulation should be similar to software regulation, considering the unique risks of each technology. Various government bodies, including Congress, the FDA, and state lawmakers, are working on these regulations from different perspectives, making it complex to track. Over half of U.S. states have introduced or passed bills addressing healthcare AI, emphasizing the importance of monitoring evolving laws and policies. The authors plan to continually update this comprehensive guide as the regulatory landscape develops. (Second Opinion)
The FDA's new Prescription Drug Use-Related Software (PDURS) framework is a significant development in U.S. healthcare, designed to integrate software with prescription drugs and enhance their clinical value. During a recent webinar, Jonah Comstock of pharmaphorum discussed the implications of this framework with industry experts Marty Culjat from EVERSANA and Edward Cox from Pfizer. This framework is expected to transform pharmaceutical manufacturing by enabling companies to develop software that improves patient outcomes and drug efficacy.
According to AHIP, a recent Wall Street Journal article presents a flawed and outdated perspective on Medicare Advantage (MA) chart reviews and health risk assessments. HRAs, endorsed by the Centers for Medicare & Medicaid Services (CMS) as best practice, help MA plans identify chronic conditions early and support patient health. Despite claims of overpayment, AHIP emphasizes that diagnoses from HRAs represent a minimal portion of MA spending and are subject to stringent CMS requirements. Moreover, recent CMS reforms and audit regulations further enhance oversight and accuracy of MA payments, which continue to outperform fee-for-service Medicare in reducing improper payments.
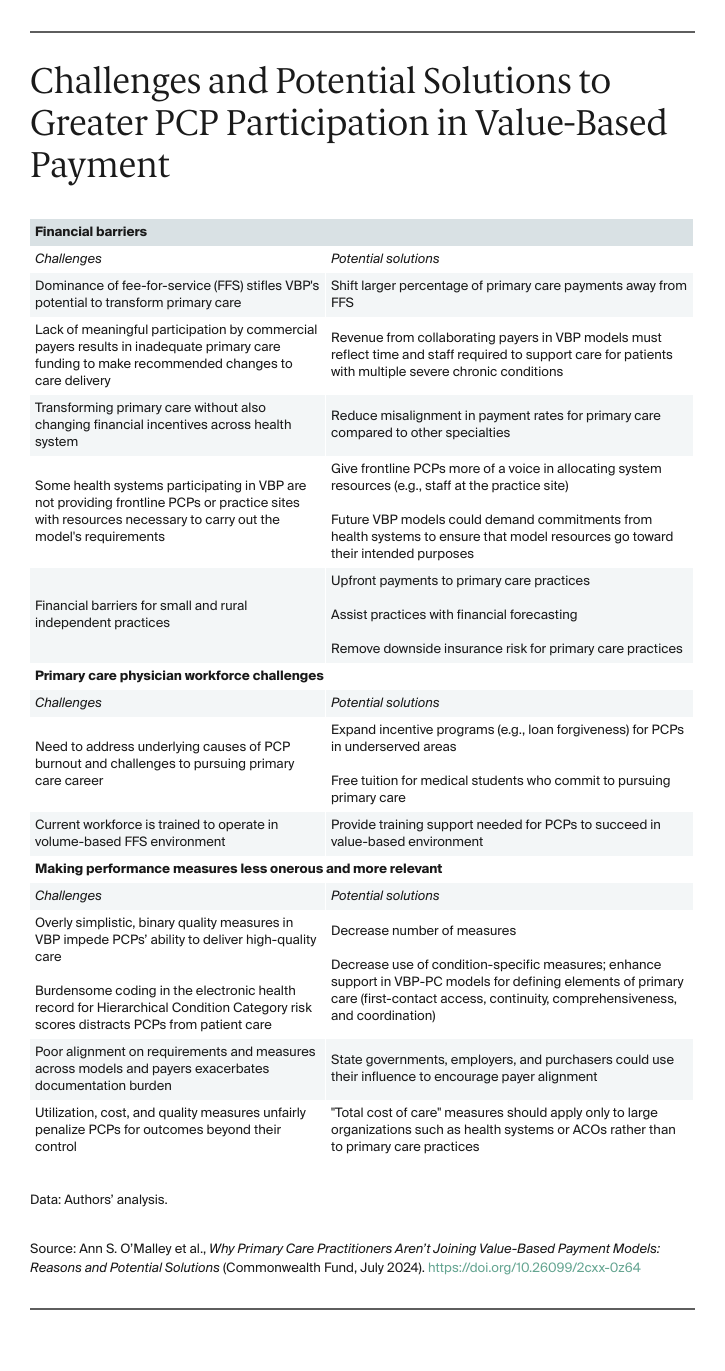
A recent issue from The Commonwealth Fund explores why most primary care practitioners (PCPs) avoid value-based payment (VBP) models despite numerous federal and state initiatives. Key reasons include financial barriers, workforce shortages, and inadequate performance measures (see below). To encourage PCP participation, the report suggests upfront payments, investment in the primary care workforce, and improved performance metrics focusing on access and continuity rather than condition-specific metrics. These changes aim to shift from fee-for-service models, promoting better-quality care and comprehensive primary care services.
“A 2022 survey found that just 46 percent of primary care physicians reported receiving any value-based payments. The smaller, independent, and less-resourced practices that serve 39 percent of traditional Medicare beneficiaries are the least likely to apply to VBP models...”
Community Voices
Commentary, opinions, and events across the [kidney] care community.

At the second biannual Samoa Kidney Conference, Acting Prime Minister Tuala Iosefo Ponifasio highlighted the escalating costs of kidney disease treatment, which have tripled over the past twenty years— from 16 dialysis patients in 2004 to 250 last year. He commended the Samoa Kidney Foundation and partners for their excellent dialysis services but stressed the need for more effective strategies to reduce the incidence of Non-Communicable Diseases (NCDs) and kidney failures. The conference aims to strategize on improving NCD policies and interventions, featuring insights from international health experts and emphasizing collaborative action to enhance health services and early detection.
In a recent piece for Forbes, SCAN Group CEO Dr. Sachin Jain highlighted the vital role of insurance brokers in promoting positive health outcomes. Brokers, trusted members of their communities, help clients navigate complex Medicare Advantage plans, ensuring access to necessary medications and healthcare services. Beyond plan selection, brokers assist clients in accessing care and connecting with social services, often providing direct support. Jain argues for officially expanding brokers' roles to include healthcare navigation, advocacy, and promoting healthy behaviors, leveraging their community trust and expertise.
Sami Inkinen, Founder and CEO of Virta Health, shared his thoughts about a Fortune article discussing the use of GLP-1 drugs like Ozempic and Wegovy for weight loss. He highlights that while pharma companies and sponsored doctors push for long-term use of these drugs, real-world data shows less than 30% of people stick with them for even a year, leading to weight regain. He points out that Virta Health has published evidence showing sustained weight loss through nutritional methods alone. He points out that while GLP-1s and bariatric surgery are valuable tools, the most sustainable solution to obesity and type 2 diabetes is a healthy diet.
Scott Nelson, co-founder and CEO of FastWave Medical and founder of Medsider, shared insights from five medtech startup CEOs in his article for MD+DI. They explore unconventional strategies that have proven successful in the challenging medtech industry: (a) leveraging risk-reward sharing partnerships to foster innovation, (b) adopting a lean executive model focused on near-term milestones, (c) integrating patient experiences at the board level to enhance product relevance, and (d) pursuing cross-industry collaborations for product validation and additional revenue streams. (MD+DI)
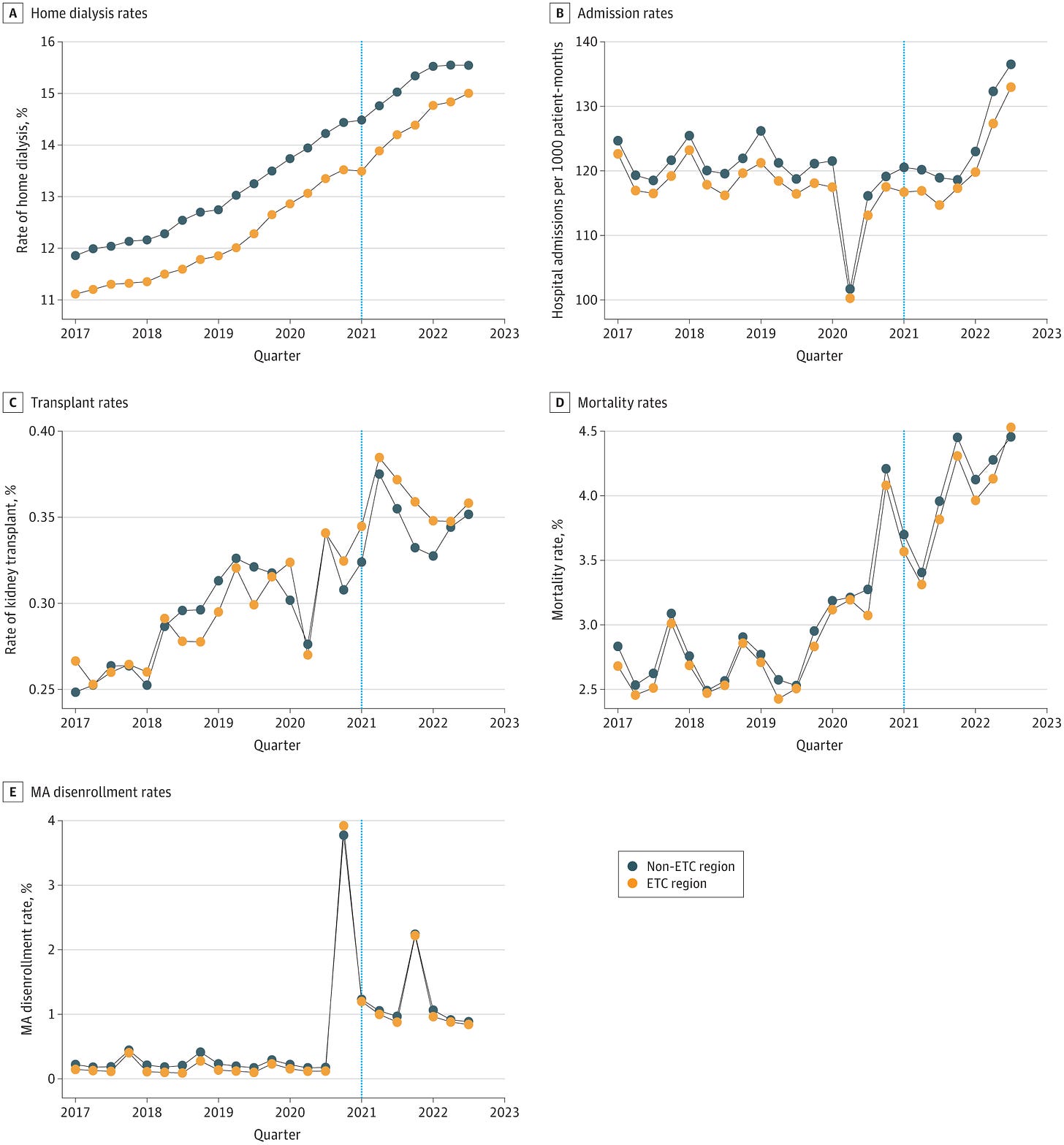
Dr. Amber Paulus wrote about the implications of market consolidation in the healthcare sector, specifically regarding the ESRD Treatment Choices (ETC) Model, which began on January 1, 2021. A recent study found that the ETC model had no significant impact on home dialysis and kidney transplant rates among patients with kidney failure. The results suggest that improvements reported by CMS may be driven by the standardized care practices implemented by the two large parent companies dominating the market, rather than the ETC model itself. This standardization ensures consistent care across all facilities, potentially masking the specific effects of the ETC model. Additionally, policy changes and reimbursement adjustments have made home dialysis more financially attractive, further influencing market behavior.1
DaVita has appointed Madhu Narasimhan as Chief Information Officer, where she will drive technology innovation and oversee the implementation of the cloud-based patient data platform, Center Without Walls. CEO Javier Rodriguez stated that under Narasimhan's leadership, the company aims to accelerate its digital transformation and enhance patient-centric care through a robust technology platform. Narasimhan brings nearly two decades of experience in integrated technology and strategic delivery, having previously led innovation at Wells Fargo and technology at Kaiser Permanente.
Beth Shanaman, Nutrition and Fitness Manager at Northwest Kidney Centers, received the 2024 Puget Sound Business Journal's Health Care Heroes Award for her exceptional contributions to nutritional education and advocacy for kidney disease patients. In her acceptance speech, Shanaman highlighted the importance of respecting patients' cultural preferences and values in their diets. She expressed pride in leading a team of 26 dietitians who prioritize understanding and meeting patients where they are, ensuring they don't feel deprived of the foods they love. Congratulations, Beth — for your dedication and all you do for patients!
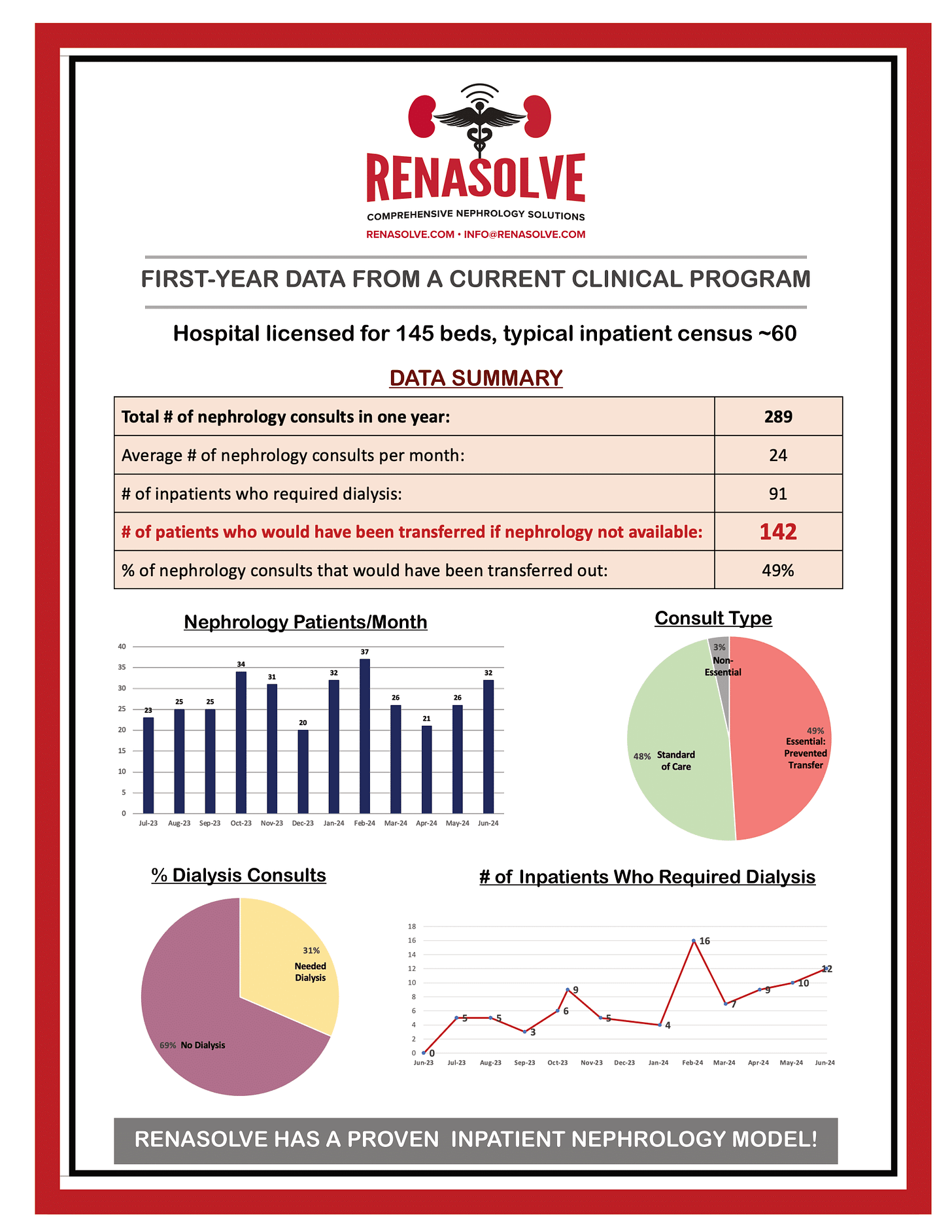
Dr. Jimmy Thomas, CMO at Renasolve, announced impressive results from their inpatient tele-nephrology and dialysis program at Randolph Health in Asheboro, NC. Over the past year, the program successfully treated 142 patients who would have otherwise been transferred to a tertiary facility. This achievement highlights the effective collaboration between Randolph Health and Outset Medical, showcasing the potential of tele-nephrology to provide high-quality care and improve patient outcomes locally. Great work, Jimmy and team!
Providers in rural and underserved areas are lobbying for long-term reimbursement certainty for telehealth, which has become essential for their operations. While recent advances in telehealth reimbursement are promising, industry executives are hesitant to make further investments without long-term predictability. Carrie Cochran-McClain of the National Rural Health Association emphasized the need for stable policies to support significant investments and the transition to telehealth beyond the end of the year. (Modern Healthcare)
A Closer Look
Dive deeper into a few headlines to see why they matter and what’s next for the space.
1. FTC's Antitrust Probe into Major Dialysis Providers
The FTC has launched an antitrust investigation into Fresenius and DaVita to determine if these companies are engaging in anti-competitive practices by restricting physician mobility and limiting patient treatment options, including home dialysis. With these two companies controlling 80% of U.S. dialysis clinics, the investigation could lead to significant changes in the dialysis market and patient care. This probe highlights the broader issue of non-compete agreements in healthcare, which critics argue stifle competition and limit patient access. The FTC's final rule banning most non-compete agreements, set to take effect in September, could further reshape the landscape for physicians and patients alike. Read more.
2. Patient Perspectives on Dialysis: Survey Insights
A recent survey of over 150 dialysis patients, sponsored by Renalogic and Lyfebulb, provides crucial insights into the dialysis experience. The findings highlight significant challenges, with 62% of patients experiencing unplanned dialysis starts and 50% expressing dissatisfaction with care coordination. Safety concerns are prevalent, with 84% witnessing serious medical events during dialysis sessions. Financial burdens also weigh heavily, as many patients face out-of-pocket costs exceeding $10,000 annually. The survey underscores the emotional toll of dialysis, with patients frequently feeling tired, anxious, and weak. These insights emphasize the need for better patient care and support systems. Read more
3. AI Regulation in Healthcare: Navigating New Policies
Christina Farr and Randi Seigel from Second Opinion detail how U.S. policymakers are working to regulate AI in healthcare, balancing its promises with the need to prevent potential harm. The American Hospital Association emphasizes that AI regulation should be specific to the unique risks posed by different technologies. Various government bodies, including Congress, the FDA, and state lawmakers, are actively shaping these regulations. Over half of U.S. states have introduced or passed bills addressing healthcare AI, highlighting the importance of monitoring evolving laws and policies to understand their impact on the industry. Read more
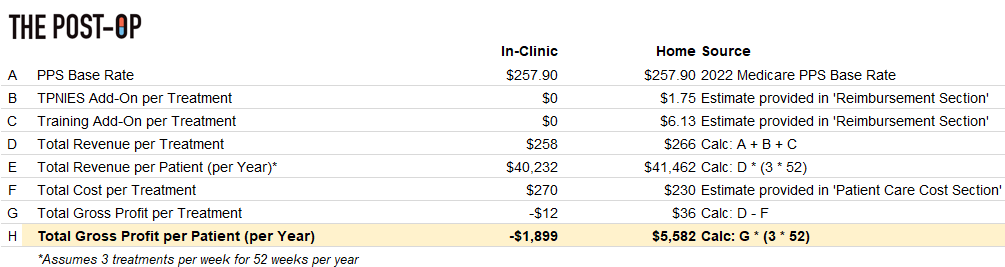
Visual of the Month
Pictures say a thousand words. What does this analysis of the business case for new dialysis devices tell us about the need for reimbursement reform in the Kidneyverse? In the years since launch, only one device (Tablo) has been approved for the TPNIES add-on payment from CMS.
For those who might have missed it, we just hosted our first Signals Live event where we touched on the topic of reimbursement barriers to device innovation. My thanks to Terry Litchfield for raising this point — and we hope to see you at the next one!
Open Roles
Here’s a list of high priority open roles across the Kidneyverse. Send me a message if you want to get in touch with these companies and hiring teams.
Renvio — Clinical Education Specialist: The Clinical Education Specialist is a bridge between the healthcare industry, Visonex, and the clients. This role requires extensive industry knowledge, including clinical practices and workflows.
AstraZeneca — Global Medical Head (Cardiovascular): As the Global Medical Head, CV, you will shape product and disease area strategy, build our capability, drive product launches and life cycle management, provide strategic direction for evidence generation, education and publication, and engage extensively externally to further the scientific leadership of AZ.
Monogram — Program Manager, Analytics: This role will be part of the Monogram Health Analytics organization consisting of actuarial, underwriting, analytics, reporting, medical economics, and data science team members.
Interwell — Director, Patient and Care Team Solutions: You will lead a dynamic team of product managers, product owners, and scrum teams. Your mission will be to ideate, design, build, and oversee a portfolio of digitally enabled services that seamlessly connect patients with clinicians, engagement specialists, primary care physicians, and nephrologists.
Mozarc — Global Sr Manager, IT Infrastructure: As part of a start-up, you will have a unique opportunity to recommend and influence solutions for the business, use your creativity and passion to drive outcomes across the organization, set direction, implement new technologies and lead the transition of IT technologies to our newly independent organization.
Keep Exploring
That’s all for this month. Thank you for being here. Please know how grateful I am for your work, interests, passions, and support for this labor of love. If you tuned in to this month’s Signals Live event on LinkedIn, please share any feedback on how we can make the next one even better.
As always, let us know what’s on your mind, who we should know, and what we should explore next.
— Tim
Want to support my work?
ESRD Treatment Choices (ETC) Model — CMS.gov

![Signals From [Space]](https://substackcdn.com/image/fetch/e_trim:10:white/e_trim:10:transparent/h_72,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F2efc1ef1-ba0b-4ca3-b9f6-a9a790da4b38_1344x256.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/w_36,h_36,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2Fa4736f49-6a20-4fd6-a3de-d48cb4b105f2_375x375.png)