Expert Q&A: Patient-Centric Kidney Innovation
How 7 patient advocates think about progress, pitfalls, and potential in this space
Welcome to a special edition of Signals Expert Q&A, the series that that asks industry leaders to weigh-in on pitfalls, progress, and potential in their respective areas of expertise in the Kidneyverse.
Today, our spotlight shines bright on patient-centric transformations in kidney care. This session brings together an extraordinary group of patients and care partners—true pioneers who have turned their personal struggles into a greater purpose for helping others.
We’re about to dive deep with seven trailblazers whose lives and efforts have been pivotal in shifting several paradigms within kidney care. From grassroots advocacy to groundbreaking involvement in clinical research, they've not only witnessed but have also sparked the evolution of care strategies that put patients at the forefront. This conversation is shaped by decades of personal experiences, and the relentless pursuit of better lives for those impacted by kidney disease.
Join us as these champions of change discuss the hurdles they've overcome, the victories they've celebrated, and the lessons they've learned along the way. For anyone invested in the future of healthcare, this thread offers not only a blueprint for patient-centric care, but also a heartfelt reminder of why these changes matter.
Reading time: 40 minutes.
Meet our experts
Our experts represent a broad range of insights and experiences, including academia, advocacy, and industry. Today, they shape our understanding of the impacts of these care models on society, raise awareness and support at the federal level, and provide care for hundreds of thousands of lives across the country. I’m grateful for their leadership and for sharing their earned wisdom with all of us today.
Terry Litchfield, President at Access Solutions
Karin Hehenberger, President at Lyfebulb
Fred Hill, Founder at Dialysis Is Not Your Life
Christina Gilchrist, “Blind Chick” at Living on Dialysis
Michael Gilchrist, “The Caretaker” at Living on Dialysis
Jeff Parke, Operations Leader & Patient Advocate
Vanessa Evans, Director of Advocacy at Fresenius
What you’ll learn









Q&A
Q1. Current state of patient-centric kidney care. At the highest level, what does "patient-centric" kidney care mean to you as you see or experience it today?
TLDR: Our experts unanimously affirm the importance of patient-centric innovation in kidney care, advocating for a fundamental shift in how care is delivered. The emphasis is on treating patients as active participants in their care, not just recipients. This involves treating them as whole individuals, addressing both mental and physical health, and integrating their personal goals and lifestyles into treatment plans. By prioritizing patient needs and preferences, healthcare providers should focus on making treatments more accessible at home and enhancing the patient's quality of life. The goal is to transform patients from passive recipients into active partners who are empowered and informed about their care decisions, ultimately aiming to restore their productivity and normalcy in life.
A1. State of Care
Terry:
Nothing about me without me! It means that those who offer health care should stop acting like hosts to patients and their families and start acting like guests in their lives.
Karin: I believe that patient-centric care, independent of organ needs to pay attention to the patient’s needs first, while also leveraging the expertise of the provider. In the case of kidney care, we unfortunately have antiquated means of treating patients. If we put the patients first, we might be using the home more and pushing harder for returning the patient back to productivity, which always is the goal for someone living with a chronic condition. Patients do not want to be patients, they want to be people.
Fred: To me, "patient-centric" care means being treated holistically as a person, considering both mental and physical well-being, rather than just as a diagnosis. It involves actively including me in making decisions about my health and ensuring that I am thoroughly listened to during appointments without feeling rushed. It also means that my concerns are genuinely heard and addressed, with a clear explanation of my monthly lab results and the necessary actions to take if those results are not within the appropriate range.
Jeff: To me, "patient-centric" kidney care represents a holistic approach that places the patient's needs, preferences, and overall well-being at the forefront of all medical decisions and care strategies. In today's healthcare landscape, this concept extends beyond mere medical treatment to include comprehensive support systems that address the physical, emotional, and social aspects of living with kidney disease. Patient-centric care emphasizes personalized treatment plans tailored to the individual's specific health conditions, lifestyle, and personal goals. It involves active patient engagement in decision-making processes, ensuring that patients are well-informed and empowered to take control of their health. This approach also includes robust support for care partners, recognizing their vital role in managing chronic kidney conditions, particularly in home dialysis scenarios.
Q2. Current barriers to patient-centric kidney care. What do you see as the biggest barrier(s) to delivering patient-centric kidney care?
TLDR: Experts identify several critical barriers to achieving patient-centric kidney care, with the predominant challenges centered around systemic inflexibility, cost, lack of education, and insufficient patient engagement. The traditional, regimented approach to kidney care often excludes patients from active participation, with a prevailing mindset resistant to systemic change. Financial constraints are highlighted as a significant hurdle, impacting the ability to empower patients fully. Additionally, the demographic and economic diversity among patients complicates the delivery of personalized treatment, particularly in early disease stages where intervention is most effective. Other notable barriers include the rushed nature of healthcare delivery, prejudgment of patients' capabilities, and the overwhelming impact of social determinants of health. Addressing these issues requires a holistic approach that encompasses better patient education, reformed care delivery models, and broader systemic changes to ensure all patients have access to appropriate and effective treatment options.
A2. Barriers
Terry: Kidney care is very regimented, and the roles and responsibilities are surrounding the patient but not always inclusive of the patient. True patient centric care meaningfully includes the patient as part of the process of care. That step tends to slow things down as they don't always process the way providers do. The biggest barrier is the mindset that the current way of delivery is the "right" way and not enough encouragement of changing the system. At the end of the day, money gets in the way. Patient engagement costs more on the front side to end up with empowered patients who understand their disease and its treatment.
Karin: There are huge barriers in kidney care due to the demographics and the very large cost to the system. Delivering personalized treatment to all kidney patients is impossible, especially since many are not even aware of being diagnosed. The insidious nature of the condition is one of the largest barriers, especially since the earlier stages of the disease are where reversal and even prevention of costs and complications can occur. In the later stages, the bigger issues are access to home dialysis, transplantation and then care management as well as better drugs.
Fred: It’s the rush to get to the next patient to not get behind schedule. Or the physician is not concerned about the well-being of the patient, only the diagnosis. It’s when no information is given to the patient to deal with the mental, physical, and emotional distress and impact that kidney disease and dialysis has on the patients and their families.
Christina: In my opinion, the greatest barrier to patient centric dialysis is cost, although I think all of the other examples are very important as well.
Michael: Education plus time of the education, every single doctor appointment should be a sit-down analysis of all your medical results. Most kidney disease patients “crash” into dialysis but with appropriate kidney medical education from diet all the way to explaining all different forms of dialysis. The worst time to address different modalities is when someone is full of toxins and isn’t thinking correctly. I also feel that PD dialysis should be the first initial dialysis offered. When peritoneal dialysis is effective it can prepare them for other modalities and start introducing hemodialysis.
Another thing that gets in the way of effective kidney care is pre-judging of the patient. If someone would have looked outside the box and helped Christina do home dialysis at the beginning, she wouldn’t have missed 6 years of her daughter’s young life. Authorities looked at paperwork seeing that she is blind and already put in mind that she cannot do home dialysis. Do not prejudge your patients. We expect people in kidney failure to drive to the clinic, to work, pay their bills and to even vote, yet we take away the option of a certain dialysis modality.
Jeff: The biggest barriers to delivering patient-centric kidney care include: (i) access to care: geographic, economic, and logistical factors significantly hinder patients' ability to access consistent and comprehensive kidney care; (ii) awareness and education; (iii) late diagnosis; and (iv) social determinants of health (SDOH): factors such as socioeconomic status, education, and environment play a critical role in health outcomes.
Q3. Solutions: What can be done today to overcome these barriers? Who will need to be involved? What does a great outcome look like?
TLDR: To overcome barriers to patient-centric care, experts advocate for comprehensive solutions that center around patient education, involvement, and support. The proposed strategies include forming true dialysis teams where patients are actively engaged in decision-making and held accountable for their health choices, which would lead to improved outcomes and satisfaction within the shared care ecosystem. Additionally, enhancing awareness and diagnosis in early CKD stages, particularly through public campaigns and specialized tools, is crucial. In later stages, increasing education on transplantation and developing better drugs are essential. Experts also emphasize the need for government and private sector collaboration to modify healthcare guidelines and innovate with technology-based solutions. Training for healthcare providers on patient communication, alongside the implementation of more supportive community-based programs, can significantly reduce the emotional and physical burden on patients. Furthermore, proactive measures such as early prevention and comprehensive home dialysis training, supported by Medicare, could drastically change the landscape of kidney care. Engaging all stakeholders—including healthcare providers, policymakers, and patient advocacy groups—in these initiatives is vital for the success of these patient-centric care models.
A3. Solutions
Terry: A true dialysis team where the patient is educated and is included in decision making and accountable for their actions (or inactions). The benefits would be in better kidney health for patients and fewer adverse events with everyone happier in the shared ecosystem.
Karin: In the early stages of CKD: awareness of the condition, better diagnosis followed by treatment protocols. Public campaigns and addressing especially minority communities with peer-to-peer support and engaging tools could make a difference (NKF has created some good ones). In later stages we need more education about transplantation and how to ask someone to be a living donor due to the lack of supply. In parallel, there is a need for better drug development in both kidney disease as well as for maintaining transplanted organs.
I believe we need both government and private entities involved to make this shift happen, since there is a need to modify guidelines, regulatory frameworks as well as develop clever solutions that might be app based or product based.
Fred: For doctors to receive patient communication training to make the patient feel like a person and that there is a genuine concern about the health of the patient. Offering help to deal with the mental, physical, emotional, impact of kidney disease and dialysis. I believe you will see less depression and anxiety about having kidney disease and being on dialysis— and better patient adherence.
Christina: The burden on society to cover Medicare for dialysis patients is overwhelming, so early prevention must be made a priority. The fewer people ending up on dialysis, the more tax money there is to spend on other things, such as increasing staff pay to retain employees. Therefore, there would be no shortages, and any patient who wants to go home needs to be trained to do home dialysis. Their health will slowly improve over time, making them less likely to go to the hospital for minor illnesses, thus saving more money for Medicare. With these savings, funds could be allocated to pay for nurses to go to the homes of patients who cannot physically or mentally perform their own home dialysis, to administer it there. This would lead to them becoming less sick over time, saving more money for Medicare in the long run. The time frame for this is uncertain since working with the government takes time. However, if we start with actionable steps now, such as training patients who are able to go home on dialysis, this will offset our current Medicare situation. I truly believe that with more advocacy, we could see a significant change in the percentage of patients going home within 4 to 5 years.1
Michael: Education and preventative care. During preventative care, educate about modalities and have the patients talk to a kidney advocate — and not a medical kidney advocates— a normal everyday person kidney advocate that can talk to them one on one about what to expect during this process. There should be neutral funding for someone that can come in and explain to them about all the different modalities and different machines, we are partial and like the machine we are using but that doesn’t mean we shouldn’t know about the other home machine options. Just like when someone goes to court, and they have an interpreter if they don’t understand the same thing should be offered to kidney patients because what they don’t know is so huge.
Also have them join a support group and I don’t care which one, I am particular to my support group LIVING!! on dialysis but just join one, at this time in their lives they are thinking they are alone when there are hundreds going through the exact same process they are in.
Jeff: Expanded access to care. Enhanced patient education and awareness. Promotion of early detection. Better ways to address social determinants of health. Development of community-based programs that provide resources and support to address the broader social factors affecting kidney health.
Getting all stakeholders involved: healthcare providers (nephrologists, primary care physicians, nurses, dieticians), healthcare organizations and clinics, policymakers and government health agencies, patient advocacy groups, community organizations, technology developers and telehealth providers.
A great outcome in patient-centric kidney care would manifest as improved patient outcomes, enhanced patient satisfaction, reduced healthcare costs, equitable access to care, and empowered care partners.
Q4. Policy: What policy changes or initiatives do you believe are necessary to improve patient-centered care in kidney health? What should advocates know, and policymakers act on?
TLDR: Experts call for substantial policy reforms to elevate kidney care to the priority level of diseases like cancer or heart disease. They advocate for a "re-branding" of kidney care to attract political support and influence policy changes, including legislation that protects home dialysis, improves patient safety, enhances organ procurement and transplantation, and updates physician fee schedules. Additionally, more nuanced, tiered approaches that cater to patients' diverse needs and circumstances are needed, emphasizing community-specific outreach over broad national programs. Mental and emotional support for patients living with kidney disease is seen as critical, with an emphasis on addressing the associated depression, anxiety, and social isolation. Incentives for home-based care are also highlighted as a policy priority, to reduce costs and provide compensation for care partners, including spouses. Policy changes should also focus on increasing funding for research, supporting care partners, expanding telehealth services, and strengthening healthcare equity programs to address social determinants of health effectively.

A4. Policy
Terry: Somehow kidney care has not been one of the highlighted diseases like cancer or heart disease. We need to collective "re-brand" kidney care and engage politicians in that re-brand effort. Current bills include protecting home dialysis; patient safety bills; organ procurement / transplant bills; updating the physician fee schedule so my doctors stay in business, to name a few.2
Karin: We need more tiered approaches that cater to patients where they are, versus only national programs that do not seem to resonate with all patients. Reaching patients in their communities versus blanket statements is what patients are asking for (e.g. churches, barber shops, etc.). For the early-stages of CKD, prevention needs to have happened already prior to diabetes diagnosis (leading cause of CKD, and efforts including addressing food deserts and even healthcare deserts are top priorities).
Fred: I believe that more focus should be on the mental and emotional well-being of the patient. Living with kidney disease and being on dialysis affects the patients and their families. Depression, anxiety, suicide and loss of social life are rising in the kidney community.3
Michael & Christina: Give an incentive for patients to go home and do their own medical care. Dialysis is billed as dialysis, and it costs us the same to go in center as it is to stay home. We do not have a team of techs or nurses, plus taking up chair time— it is just me and my wife doing home dialysis, yet we pay the same amount. One, there should be an incentive for the clinic to have people doing dialysis at home, but also for the patient and care partner. Christina and I are married, and she does nocturnal home hemodialysis for 7.5 hours 4 times per week, with no financial help. There are programs out there to help pay your care partner, but that person can’t be a spouse as a care partner. It is pathetic: in order for me to get compensation for my time administering my wife’s dialysis, I would have to divorce her.4
Jeff: To improve patient-centered care in kidney health, the following policy changes and initiatives are necessary: increased funding for kidney disease research and prevention: support for care partners: passing of legislation like "Marie's Bill" — this is a bill that I provided to our Florida state senators. We must expand telehealth services by removing barriers to telehealth adoption by ensuring reimbursement parity with in-person visits and investing in the necessary infrastructure to support remote care. We must also strengthen healthcare equity programs by implementing policies that address social determinants of health, ensuring all patients have access to nutritious food, safe housing, and necessary healthcare services.5
Q5. Future directions: Looking ahead, where do you see the most important priorities for patient-centric innovation?
TLDR: Experts emphasize the critical role of patient voices in shaping insurance coverage and policy, pushing for faster approval and reimbursement processes to expedite access to new treatments. There is a strong call to increase the supply and improve the management of transplantation through xenotransplantation and enhanced post-transplant care. Additionally, innovations in home dialysis technology, better training for care providers, and patient education are seen as pivotal areas for development. Advocates also highlight the need for lighter, more portable dialysis machines to enhance mobility and quality of life for patients. The overarching vision is a more integrated, patient-centric approach that reduces barriers to treatment and fosters a higher quality of life for those affected by kidney disease.
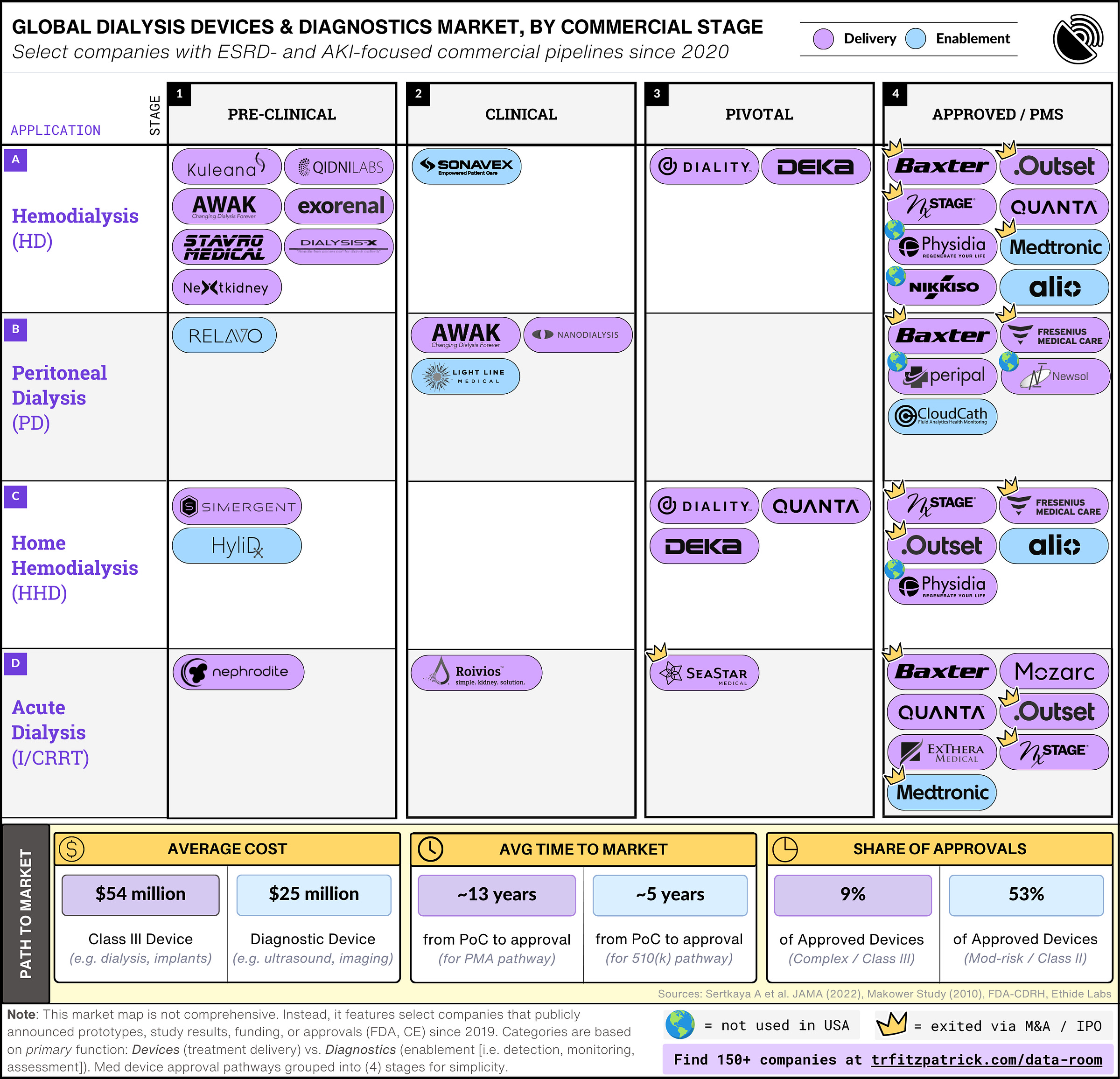
A5. The Future
Terry: Kidney patients were critical in the early years of getting insurance coverage for dialysis. We have recently started with more patient advocacy and that needs to be fostered, nurtured and funded to create a revolution. New drugs and devices in kidney care get buried at regulatory levels (for example the new drug and device innovation projects are not long term). We complain about the lack of innovation, but the programs rolled out do not do enough to get exciting new things into the hands of patients. Long approval times for new drugs or devices mean that some patients die waiting for access to a technology that is around, maybe just not approved or reimbursed... Congress, HHS, FDA, and CMS need to break down the barriers that slow down technology. Speed up the processes all along the product life cycle and ensure reimbursement is there to help new innovations get to patients at warp speed. Imagine that world that benchtop to bedside in the dialysis unit or at home is a matter of months not years (or never).6
Imagine that world that benchtop to bedside in the dialysis unit or at home is a matter of months, not years (or never). — Terry Litchfield
Karin: Personally, I am most excited about transplantation:
increasing the supply by exploring xenotransplantation and improving the terms for living donation;
improving the drugs used for keeping the graft alive by changing the endpoints for clinical trials to reflect the longer survival of the graft, thus stimulating financing of science; and
securing adherence long term through better care management programs.7
Fred: I see great things happening. There are more innovative monitoring devices, advancements in technology for home dialysis, and more attention in kidney advocacy. If we get it right, there will be fewer horror stories about kidney disease and more confident patients living a quality level of life with kidney disease and on dialysis.
Christina: I think that by focusing on empowering patients and ensuring they are fully informed from the start about their dialysis options, we can make significant progress. Patients should meet with a kidney advocate to discuss peritoneal dialysis, in-center hemodialysis, and home dialysis. It's crucial that care partners are involved and all family questions are addressed, as they are just as important to the decision-making process as the patients themselves.
Once patients are well-informed, the next step is thorough training. This requires a specialized group of nurses, which is where investment is needed. We need to revitalize the dialysis community and make it a thriving career choice again. Respecting patients' personal choices is key to improving care.
I am incredibly passionate about home dialysis—I am alive today because of it. For years, I wasn't given the opportunity to explore my modality options. When I decided to pursue home dialysis, I had to seek out the solutions myself. It's thrilling to see that the future is changing and that we are learning from those who have gone before. There's something uniquely impactful about patients talking to each other, and if in-center patients could see how those of us at home are living, I believe they would all choose home dialysis. With careful planning and thoughtful implementation, hopefully, this can become a reality for more patients.
Michael: More patient advocates helping advance home dialysis modalities. I love the fact that we can travel the country showing people how to do home dialysis, but I will say that traveling is not the easiest, I am still having to lug around a 100-lbs machine and that doesn’t include all her other medical. We must make advancing kidney dialysis modalities number one. In the 1950’s the space program had computers the size of houses, no one had a home computer but now with advancements every single person carries a supercomputer in their pocket and sometimes on their wrist, but dialysis was first used in the 1940’s and advancements have been made but still using big machines that weigh quite a bit. It is time to have dialysis machines that fit in our pocket.
Jeff: The most important priorities and potential for patient-centric innovation in kidney care include expanding and improving at-home dialysis options, making them more accessible and user-friendly, advanced technology and devices, patient advocacy and empowerment, transplant innovations, and integrated care models.
Q6. Story time! I’d love to hear about a personal story or conversation that left a mark or fuels your work today?
Terry: My pet peeve is when a provider asks if we have any questions after dropping a new diagnosis/bad news/etc. No, I have no questions because I have no idea what question to ask...tell ME what we should be asking you. Look me in the eye when you are talking to me--don't talk to the computer screen where you are trying to write this down and don't talk down to me when you are rushing around the dialysis unit making rounds. Sit down and talk to me; ask me questions and listen to my voice.
Karin: I had my first kidney transplant on March 12, 2009, and from all perspectives, it was a great success! It allowed me to go on to have a pancreas transplant (without a normal kidney function, it would have been hard to go through that very tough surgery), venture out to start a company (Lyfebulb), and conceive a child. Those were the highlights.
But let us not forget everything else that this kidney allowed me to do. First of all, it let me live. Without it, I would most likely have been on dialysis within a year or so, and the life expectancy of a diabetic person on dialysis is less than 5 years. I also traveled to many interesting places, got married, enjoyed new and old friendships, and participated in sports such as tennis and running during these 14 years. So, to start, I want to thank my donor, my Father, for this life-saving gift.
However, for the past 3 years or so, my kidney has been in steady decline… Continue reading Karin’s story on her blog here.
Fred: Going on dialysis was hard on me and my family. I went through depression, anxiety, grief, loss of social life, marriage problems, loss of confidence and truly thinking my life was over. Not just me but my wife and son as well. We didn't know what to do or where to go for help. If there was some type of kidney disease or dialysis mental health support available for me and my family our live would have been so much better.
Christina: Summarizing my medical history can be quite a challenge—it tends to leave people wide-eyed and exclaiming, "You went through what?!" But, here it is, laid out straightforwardly, as Michael would recount it, with just the facts.
I was diagnosed with kidney disease as a young teen and was assured it wouldn’t impact me significantly until much later in life. However, during pregnancy, I missed signs of toxemia, leading to seizures that caused temporary blindness and ultimately resulted in kidney rejection. My brother generously donated a kidney to me, but tragically, I rejected it after just a year and a half. Following that, I spent about 5.5 years on in-center dialysis, all while raising my young son as a single mother.
A second transplant came from a deceased donor, around the same time Michael entered my life with some rather questionable pickup lines that, for some reason, worked. Yet, history repeated itself about 1.5 years later when I started rejecting this second kidney. Despite our best efforts, throwing every possible medication at it, even chemotherapy, we had to let the kidney go, and I underwent surgery to remove it.
Refusing to be hindered by my poor eyesight, which initially disqualified me from home dialysis, I began doctor shopping. I was determined to find a way to do peritoneal dialysis (PD) at home. Eventually, I reconnected with my original nephrologist who supported my decision to start PD, which I managed with special techniques adapted for my limited vision.
Life with Michael meant adapting every aspect of our lives to accommodate my dialysis needs. We managed PD on road trips, vacations, and even on the back of a motorcycle, using solar panels when dry camping. Although PD was initially effective, allowing us to get engaged and then married, it eventually ceased due to abdominal adhesions.
Switching gears, we trained for home hemodialysis, which we started on Christmas 2021. Michael, with no medical background but a keen interest fueled by his desire to keep me healthy, learned everything he could about the process. Frustrated by the negativity we encountered in existing support groups, we started our own, called "LIVING!! on Dialysis," quickly gaining recognition as "Blind Chick Living and The Caretaker."
Through it all, I’ve had every type of dialysis access imaginable and even underwent heart valve replacement surgery, which revealed a calcified pericardium requiring the surgeon to delicately peel my heart like a potato. We’ve traveled extensively, advocating for more funding for kidney disease and demonstrating that life on dialysis is not only possible but can be full of adventure and significant milestones. Celebrating my 40th birthday, watching my son graduate and go to college, and becoming a grandma are just a few highlights of my journey.
In my life, the mantra has always been, “Don’t tell me I can’t! Show me how I can!” And truly, each chapter of my story is more astounding than the last.
— Christina Gilchrist
Michael: Doing home dialysis, you are healthier and will in most cases feel better, which means you heal from surgeries better, and you spend less time in the hospital. Christina had open heart surgery. Her healing from this huge surgery had a lot to do with her health and home dialysis. Her body is so used to doing slow and easy home dialysis that her body was not use to the dialysis she was receiving in the hospital. She was slowly putting on more and more water weight due to not receiving as effective dialysis as she would get at home. We begged the hospital to allow Michael to bring in Christina’s dialysis machine so he could take off all needed fluid a lot quicker than any machine they had in the hospital. Since I am not a medical professional, I was not able to perform her medical care, which is the opposite of how we should be thinking— if there is a better form of care, let the patient have it. Because Christina was healing well from open heart surgery, we were able to convince her team to let her do the rest of her healing at home where I could do dialysis on her. During her time in the hospital Christina slowly put on over 20-lbs of fluid. Michael was able to take her home and do back-to-back treatments removing 20-lbs of fluid in less than 2 days.8
Jeff: Our decision to transition to home hemodialysis was a significant turning point. It promised greater flexibility and comfort, allowing me to receive treatment in the familiar surroundings of our home. However, this transition was not without its challenges. Marie had to undergo extensive training to learn how to operate the dialysis machine, manage potential complications, and maintain strict hygiene standards. The responsibility was immense, but she embraced it with unwavering commitment.
One particular incident stands out vividly in my memory. During one of our early home dialysis sessions, I experienced a sudden drop in blood pressure—a common but frightening complication. Marie remained calm and composed, quickly implementing the emergency protocols she had learned. Her ability to manage the situation effectively not only stabilized my condition but also reinforced my trust in her capabilities as a care partner. This experience underscored the critical importance of having a well-trained and supported care partner, especially in the home dialysis setting.
This personal journey has fueled my advocacy for care partner recognition and support. The challenges we faced and the critical role Marie played in my treatment have reinforced my belief that care partners must be formally recognized and adequately supported. This is why I am a strong advocate for "Marie's Bill," which seeks to address care partner burnout by providing financial compensation and establishing support mechanisms for those who dedicate their lives to caring for loved ones with chronic conditions.
Moreover, interactions with healthcare providers have often highlighted misconceptions about the role of care partners. Many providers view care partners merely as auxiliary support, overlooking the comprehensive and multifaceted nature of their contributions. Care partners are not just helpers; they are integral members of the healthcare team, providing essential care that directly impacts patient outcomes. Recognizing and integrating their insights and experiences into the healthcare process can significantly enhance the quality of care provided.
Q7. What’s something people should know about being a patient or care partner that they may not know?
TLDR: Experts highlight some lesser-known yet significant aspects of being a dialysis patient or care partner. Dialysis affects not only the patient but their entire family, adding complex health care routines on top of normal life challenges. Education and understanding of treatment options like home dialysis are crucial, as they significantly improve quality of life by alleviating common dialysis-related symptoms. Care partners, often overlooked, play a critical role in the patient's care regimen but face immense personal and professional sacrifices. Their integration into the patient's medical decisions, adequate training, and empowerment through patient advocacy are seen as pivotal for improving both patient and care partner experiences. Furthermore, there is a call for greater recognition and support for care partners, who need to be considered as integral members of the health care team, deserving of both recognition and compensation for their efforts.
A7. Did you know?
Terry: Dialysis is not our life; it is our family life, because without it there is no life. Patients and their care partners have all of the same things that real world people experience. Just add on dialysis, treatment, or other health care issues and it can be really tough. Sprinkle in the social determinants of health (e.g. income levels, age, education, race, ethnicity) and it can be overwhelming. Lend a hand, offer help or just share a kind word or deed.
Karin: Transplantation is not a cure, but a continued treatment for end-stage disease and must not be seen as anything else until the drugs we need enable us to live without fear of complications and return to graft failure within our lifetime. However, the difference between dialysis and transplant is immense and we need to increase the pool of organs available to those on the waiting list and beyond.
Fred: Depression and anxiety in kidney disease and dialysis patients goes unnoticed. Mental health is a real challenge. Many patients have to stop working and experience financial hardship, lose confidence, marital issues, loss of social life, etc.
Christina: First, I would love to sit down with every single person, healthy or not, in this world and tell them that high blood pressure and diabetes are the two leading causes of kidney failure. When you go to your doctor’s appointments, make sure to check these every single time. If someone says your blood pressure “just runs high,” go to a different doctor. I would also love to explain to anyone who will listen that a healthy human gets 168 hours in a week, whereas a human going to in-center dialysis only thinks about getting through 9 to 12 hours a week. That itself should explain why these patients are so miserable. These patients have to go home and recover for hours after a treatment. That is not a natural process for the human body. The machines in-center are run way too fast. They are sucking off fluid way too quickly, leaving these patients dehydrated, exhausted, frazzled, sometimes in a brain fog, nauseous, sweaty, feeling like you’re going to pass out, with cramps in your body everywhere. These are just some of the torturous side effects of dialysis.
Going home on dialysis, each patient receives their own machine, therefore they can choose to do as many hours of dialysis as they would like with their care professionals' team. Doing more dialysis is key for a person’s body when a kidney no longer works. People don’t usually understand that the kidney produces urine and so, over time after being on dialysis, some people for a long period of time, some people for a short period of time, you stop urinating completely. Also, your kidney is responsible for taking care of your potassium levels, phosphorus, and others. Therefore, the renal nutrition comes into play as a necessity, meaning you cannot get your potassium too high or too low; hence heart problems.
When a patient goes home, they are cleaning their blood more thoroughly therefore toxins are not building up to such an overwhelming number, meaning a lot of those side effects go away. Since being home myself, personally, I do not have the majority of those side effects anymore, including after I am done with dialysis. I have no recovery time. I truly can go and live my life. Therefore, I live by the motto, “I don’t live to do dialysis; I do dialysis to live.”
Thank you truly for this opportunity to be a part of this Q&A. Thank you for what you are doing. What you are doing is truly going to save millions of lives. Thank you for caring. (author’s note: ❤️)
Michael: When someone looks at Christina, I want them to be in shock every single time when she tells them she is on dialysis. I want Michael and Christina to be the goal of what kidney disease can be. Is it a lot? Absolutely. But we only live once, so what is the point in doing all this to survive if we are not going to be LIVING.
LIVING can continue while in kidney failure, with appropriate education and giving them the opportunity to thrive. The patient is not the only one that “crashes” into dialysis— the care partner does too. A care partner’s life and career is put on hold, while you can usually visually see the progress of a person’s kidney disease, the care partner often has to attempt to hold professional and personal lives together. When the patient gets healthy, medical emergencies happen less, and life can attempt to return to normal.
When Christina’s kidney failed, I had a thriving career, but it seemed like overnight, I had to give up all advancements and promotions at work. I became known as the guy who always comes in late or the guy who is always tired. However, as Christina became healthier and gained confidence in managing her medical care, especially after starting nocturnal home hemodialysis, life began to return to normal. This improvement led to one of the biggest promotions available at my job. I went from sweating under a jet, worried if my wife was going to survive, to confidently engineering for the aircraft, secure in the care I provide for Christina.
Jeff: For nearly a decade, my wife has been my unwavering care partner as I transitioned to home hemodialysis. Her dedication and commitment have been nothing short of extraordinary. She has navigated the complexities of dialysis treatment with resilience and compassion, ensuring that my health and well-being are prioritized every single day. This journey has profoundly highlighted the critical role care partners play in the healthcare ecosystem, particularly for those managing chronic conditions like kidney disease.
Despite their indispensable role, care partners are frequently overlooked in the healthcare management team. They are not formally recognized or adequately supported, both emotionally and financially. This oversight can lead to significant burnout, which not only affects the care partner’s health but also the quality of care they can provide.
Care partners play a vital role in the daily management of patients' health and are key to the success of patient-centric clinical trials. Their deep understanding of the patient's day-to-day challenges and their emotional and practical support are crucial in ensuring adherence to treatment protocols. Care partners can also act as advocates within the healthcare system, helping to navigate complex treatment landscapes and ensuring that the patient's voice is heard in decision-making processes.
However, the integration of care partners into the clinical trial process is overlooked. Trials typically focus on the patient as the primary subject and may fail to recognize the influence and insights that care, partners, bring. This oversight can result in missed opportunities to improve the trial's design and outcomes. For example, care partners might provide valuable feedback on the practical aspects of medication schedules or trial interventions, which could lead to adjustments that make protocols more manageable and less disruptive to patients' daily lives.
My personal experience with my wife's dedication as my care partner fuels my advocacy for legislative reforms such as "Marie's Bill." This bill aims to address the critical issue of care partner burnout by formally recognizing and compensating care partners for their invaluable contributions. It acknowledges the physical, emotional, and financial toll that caregiving entails and seeks to provide the necessary support to ensure that care partners can continue to provide high-quality care without compromising their own health and well-being.
"Marie's Bill," named in honor of my wife, aims to address and mitigate care partner burnout by officially recognizing it as a significant issue and ensuring care partners are compensated for their invaluable services in home dialysis care. The bill outlines a comprehensive framework that includes financial compensation, support systems, and the establishment of research initiatives to understand and address care partner burnout more effectively.
Resources & Data
I asked the experts to help us curate their favorite resources and recommendations where you can learn more about these topics. Here are their must-read deep dives:
Reports
A Strategic Blueprint for Advancing Kidney Care Quality. A multi‐stakeholder, consensus document intended to provide a near‐term roadmap on the key actions that, if undertaken through collaboration and partnership, can significantly improve kidney care quality. KCP sees the Blueprint as serving as a guidepost for public and private sector stakeholders to expand upon and/or identify their own priorities. (Kidney Care Partners)
2023 Kidney Health Initiative Annual Report. The Kidney Health Initiative (KHI) is a public-private partnership among the American Society of Nephrology (ASN), the US Food and Drug Administration (FDA), and with more than 70 member companies and organizations committed to catalyzing innovation and the development of safe and effective patient-centered therapies for people with kidney diseases.
Advocating for Health Equity in Kidney Care: An Urgent Need. Miriam Godwin’s brief calls for increased public investment in kidney health equity, closing the race and ethnicity gap in access to living donor kidney transplants, better understanding why structurally disadvantaged populations are left behind in access to deceased donor transplants, and ensuring equitable access to home dialysis success. (NKF Advocacy Brief, 2021)
2023 ISN Global Kidney Health Atlas. Closing the Gaps initiative and has been designed to assess the current capacity for kidney care across all world regions. For the first time, this edition includes perspectives on the barriers that people living with kidney disease encounter in accessing kidney care and the impacts of
kidney failure.
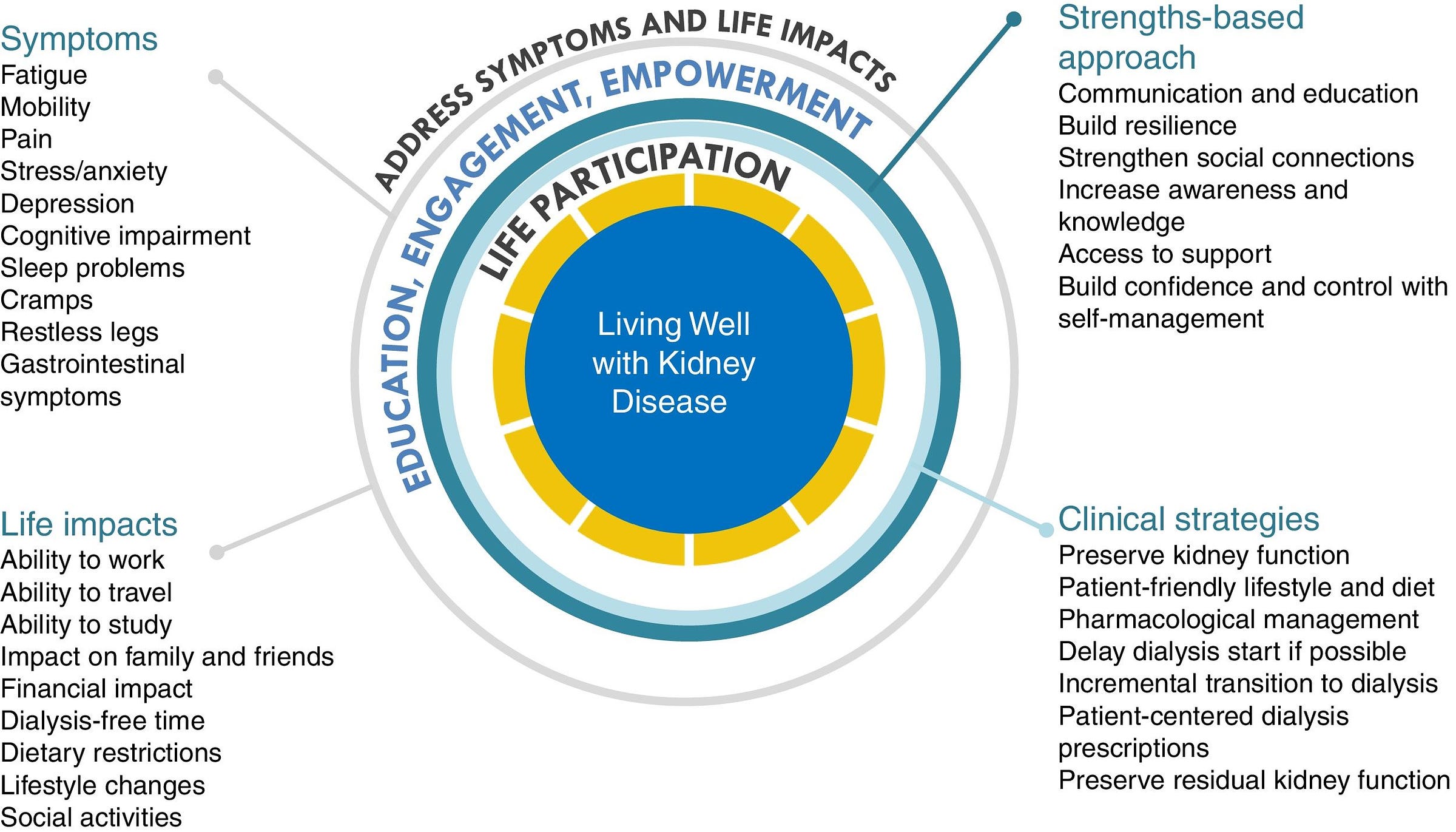
Living well with kidney disease by patient and care-partner empowerment: kidney health for everyone everywhere. The World Kidney Day (WKD) Joint Steering Committee declared 2021 the year of “Living Well with Kidney Disease” in an effort to increase education and awareness on the important goal of patient empowerment and life participation. The group underscored the need to broaden the focus on living well with kidney disease and re-engagement in life, including an emphasis on patients being in control of their care. (BJMBR, 2021)
Patient Engagement Advocacy Guide. The NKF’s Patient Engagement & Advocacy Guide provides information and resources on ways you, as a kidney patient, living donor, practitioner, or family member, can assess, articulate, and pursue the best strategies available for advocating around kidney disease awareness, prevention, and treatment.
Research & Commentary
Karin Hehenberger gave a talk at TEDxLugano on How Diabetes Patients can Transform the Diabetes Pandemic. Karin focuses on the importance of patient engagement and entrepreneurship in addressing the global crisis that is diabetes. She reveals the power of the patients’ voice in this personal, inspiring talk.
Vanessa Evans joined a webinar hosted by the Dialysis Patient Citizens Education Center titled How to be a Successful Home Patient. The 1-hour webinar covered topics like tips and trick for storing your supplies, what questions should you ask your team, and the importance of routine and organization and how to help yourself succeed.
Terry Litchfield joined a panel hosted by AAKP to talk about A New, Less Invasive Dialysis Access Option for Patients. The 1-hour event covered what an AV fistula is and how it works, a less invasive creation option vs. surgery, insights from healthcare providers and real patient caregivers, benefits and risks, and how to talk to your provider about it.
Jeff Parke has written extensively on the topics of kidney health, patient centricity, clinical trials, value-based care, and more. Find his LinkedIn articles and self-published books here.
Fred Hill wrote a piece on managing depression in patients with chronic kidney disease to slow progression. He shows how new research is further demonstrating the link between depression and progression of kidney disease, and why a value-based approach to depression screening and treatment is critical to improving patient outcomes. Fred also hosts the Dialysis Is Not Your Life channel on YouTube, which features several of our guests in today’s Q&A.
Adults Who Report Ever Being Told They Have Kidney Disease (KFF)
Thank you for tuning in for this Expert Q&A. If you find this information valuable, please consider subscribing and sharing it with peers and colleagues in your corner of the Kidneyverse today!
Keep exploring,
— Tim
HEALTHCARE STAFFING SHORTAGES AND DIALYSIS PATIENTS. (2022, November 8). National Kidney Foundation. https://www.kidney.org/newsletter/healthcare-staffing-shortages-and-dialysis-patients
RPA: Proposed Medicare Physician Fee Schedule cut should be mostly neutral for nephrology. (2024, July 19). Healio Nephrology. https://www.healio.com/news/nephrology/20240719/rpa-proposed-medicare-physician-fee-schedule-cut-should-be-mostly-neutral-for-nephrology
Shirazian S, Grant CD, Aina O, Mattana J, Khorassani F, Ricardo AC. Depression in Chronic Kidney Disease and End-Stage Renal Disease: Similarities and Differences in Diagnosis, Epidemiology, and Management. Kidney Int Rep. 2016 Sep 20;2(1):94-107. doi: 10.1016/j.ekir.2016.09.005. PMID: 29318209; PMCID: PMC5720531.
VA Caregiver Support Program — caregiver.va.gov
Gupta R, Morten CJ, Zhu AY, Ramachandran R, Shah ND, Ross JS. Approvals and Timing of New Formulations of Novel Drugs Approved by the US Food and Drug Administration Between 1995 and 2010 and Followed Through 2021. JAMA Health Forum. 2022 May 20;3(5):e221096. doi: 10.1001/jamahealthforum.2022.1096. PMID: 35977259; PMCID: PMC9123500.
First pig kidney transplant in a person: what it means for the future. Nature. https://www.nature.com/articles/d41586-024-00879-y
Maggiore, Umbertoa; Leventhal, Jeremyb,c; Cravedi, Paolob. Rethinking clinical endpoints in kidney transplant trials. Current Opinion in Organ Transplantation 25(1):p 1-7, February 2020. | DOI: 10.1097/MOT.0000000000000719
Vinson AJ, Perl J, Tennankore KK. Survival Comparisons of Home Dialysis Versus In-Center Hemodialysis: A Narrative Review. Can J Kidney Health Dis. 2019 Jul 13;6:2054358119861941. doi: 10.1177/2054358119861941. PMID: 31321065; PMCID: PMC6628511.
![Signals From [Space]](https://substackcdn.com/image/fetch/w_80,h_80,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F55686857-6b99-45a6-ac0f-09c9f023f2a0_500x500.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/e_trim:10:white/e_trim:10:transparent/h_72,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F4d588ac1-7fac-4bd4-829d-fc7b4e8f1326_1512x288.png)

![Signals From [Space]](https://substackcdn.com/image/fetch/w_36,h_36,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F55686857-6b99-45a6-ac0f-09c9f023f2a0_500x500.png)











