Across the Kidneyverse: May 19, 2024
Transplant, Vantive, Virtual Care, Dialysis Earnings & Community Voices
By Tim Fitzpatrick
Welcome back to Across the Kidneyverse, our monthly recap of top headlines, market movers, research and commentary from the past four weeks of kidney innovation. This month we’re diving further into transplant, honoring Richard Slayman, unveiling Vantive, recapping LDO earnings, running pre- and postmortems on virtual care businesses, and continuing to ask ourselves, “what do we really want out of kidney innovation — and how should we fund it?”
Have tips or feedback? Hit reply or join the conversation here.
Reading time: 25 minutes
Reminders
Kidneyverse Careers is the only place dedicated to bringing top talent and companies together across kidney care. I’m going to start sharing a few open roles per month here in the newsletter. Reach out if you want to highlight your company’s roles.📣
If you like these monthly recaps, chances are you’ll love our subscriber-only content and data. We have a lot more of it coming (videos, interviews, data, deep dives, etc.). We know a lot of you use Signals to make decisions at work, which is why we put together this draft email template you can use to ask your manager to expense a paid subscription.
The Signals Inbox is open to anyone who wants to share news, tips, and updates that belong in this monthly recap. It’s anonymous, so let me know what you’re seeing and hearing out there (especially in VBC land)!
Contents
Headlines
Here’s what caught my eye across the Kidneyverse this month, organized by topic.
Discovery & Innovation
Covering the latest in research, development, and breakthroughs.
Richard "Rick" Slayman, the first human to receive a genetically modified pig kidney transplant, has died almost two months after the procedure. Mr. Slayman received his kidney at Massachusetts General in March after he had been diagnosed with end-stage kidney disease last year. The hospital emphasized there is no indication his death was a result of the transplant. The transplant surgeon had said he hoped the transplant would function for at least two years. Over the past week, words of support have poured out from the community to honor Mr. Slayman’s bravery, selflessness, and willingness to create a brighter future for generations to come.
In April 2024, 54-year-old Lisa Pisano from New Jersey became the second person to receive a kidney transplant from a genetically modified pig. The transplant also included the pig's thymus gland, which helps the immune system fight disease. Pisano has heart failure and end-stage kidney disease, and due to chronic conditions, she was not a candidate for a heart transplant or a kidney transplant.
The team at 34 Lives just announced its rescue of the first human kidney that had been deemed not usable for transplant! The company is on a mission to decrease the number of kidneys in the US that are recovered with the intent to transplant but subsequently not used. (h/t Kevin Longino)
Toku Eyes just received FDA Breakthrough Device designation for its MyKidneyAI product that uses AI to analyze retinal images from routine eye exams to detect CKD risk in people with diabetes. (h/t Ehsan Vaghefi)
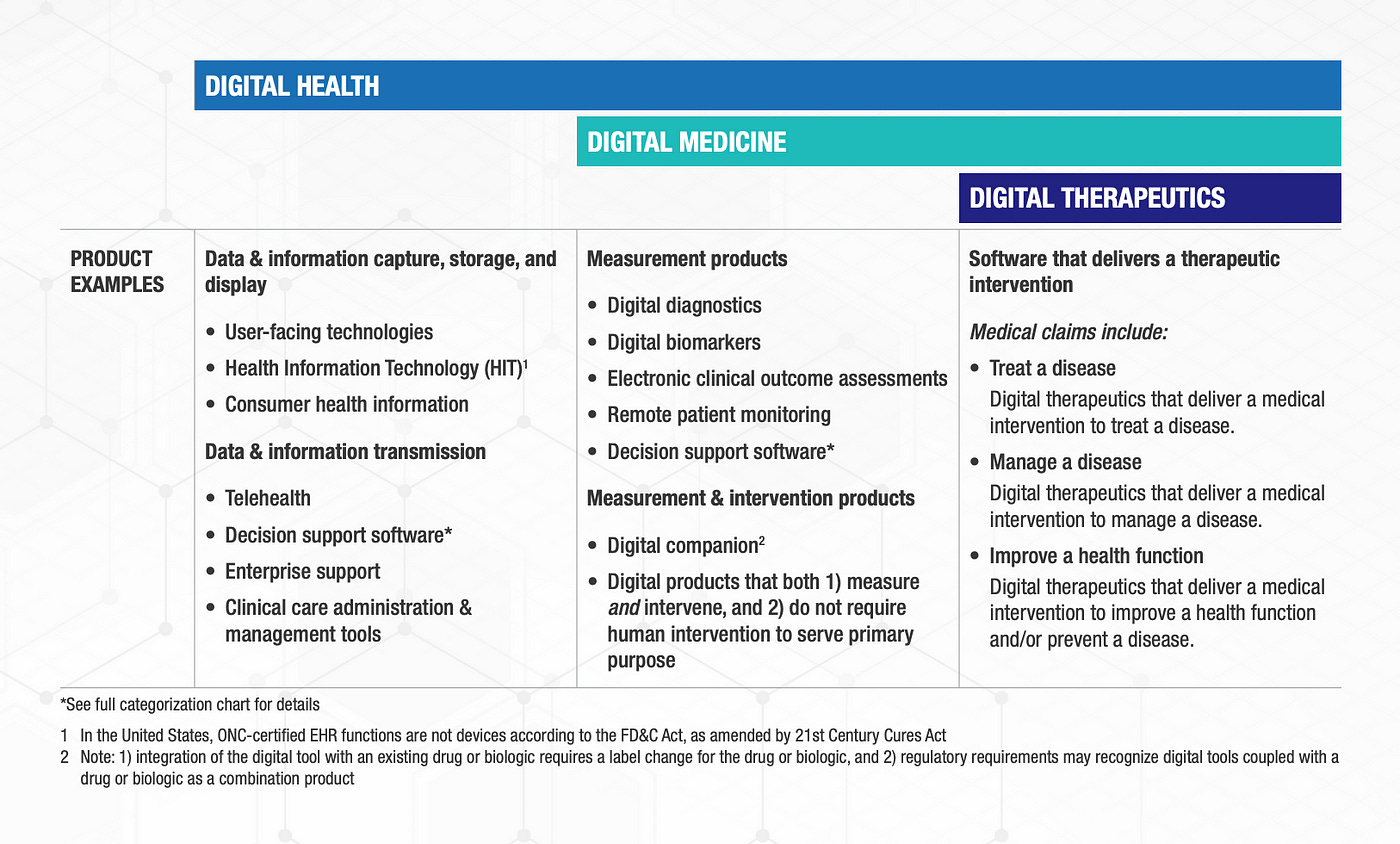
The Apple Watch AFib feature just became the first digital health product to receive FDA approval under the MDDT program. It will be used as a tool to assess atrial fibrillation burden estimates within clinical studies. (h/t Jaydeo Kinikar)
“Today is a straight-up win for all of us that believe in the promise of sensor-based digital health technologies (sDHTs) to transform the way we develop new medical products to better serve the patients our industry exists to serve. Onwards!”
— Jennifer Goldsack, CEO at Digital Medicine Society (DiMe)
Ahead of CMMI’s 2024 VBC Learning Conference last week, the NANI team shared a post on LinkedIn with a 5-page PDF that includes overview data of their optimal starts and kidney transplant efforts. In 2023, the team was able to increase their optimal start rate from 18% (Jan-July) to 71% (Aug-Dec). Kidney transplant referrals have doubled year-over-year since 2022.
Market Insight
Trends, funding updates, and industry developments.
Extending Lives, Expanding Possibilities. That's the newly announced mission for Vantive, Baxter's proposed kidney care and acute therapies company that is expected to either be spun-off or sold to private equity later this year. The Vantive logo includes a "V" motif divided into three parts to represent the innovative therapies, digital solutions, and advanced services the company delivers.
Outset Medical announced that it has received FDA 510(k) clearance of TabloCart™ with prefiltration, an innovative optional accessory for the Tablo® Hemodialysis System.
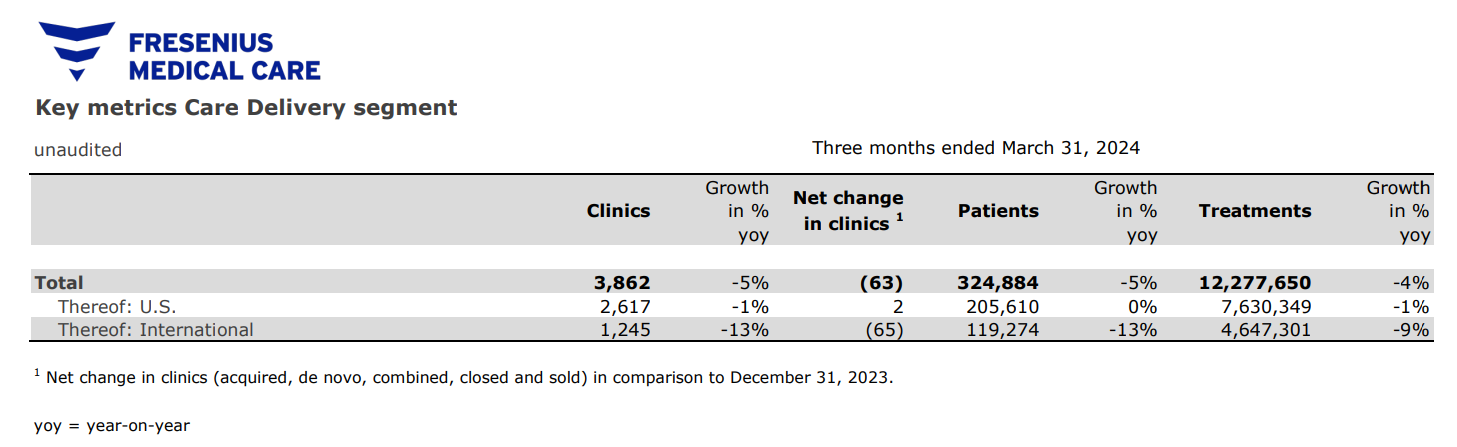
A week after reporting its first quarter results, Fresenius hosted its Annual General Meeting 2024 at the Congress Center Messe Frankfurt, Germany. This is the first AGM following the company’s change to a simpler legal form in November. It sounds like the FME25 transformation plan is working. Simply put, it’s all about delivering savings — upwards of $150 million this year, and $700 million by end of next year. CEO Helen Giza said while 2023 was about level-setting, 2024 is about building momentum with growth in both business segments: Care Delivery and Care Enablement.
Q1 by the numbers (as of March 31, 2024):
324,884 patients treated
3,862 dialysis clinics worldwide
117,128 employees globally
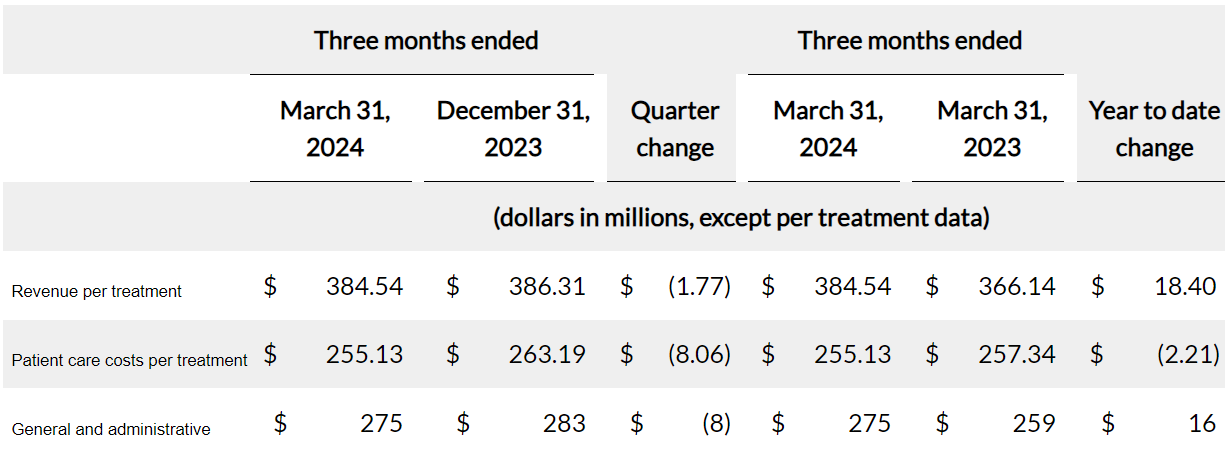
DaVita also reported its first quarter results this month. The report details key drivers of revenue and metrics in the summary table below. Note: Both FMC and DVA reported Q1 impacts from the Change Healthcare outage. DVA says it has applied for and received $472 million as of April 30 from UnitedHealth’s temporary funding assistance program, or TFAP.
Q1 by the numbers (as of March 31, 2024):
258,600 patients treated
3,092 dialysis clinics worldwide
7,151,512 treatments delivered
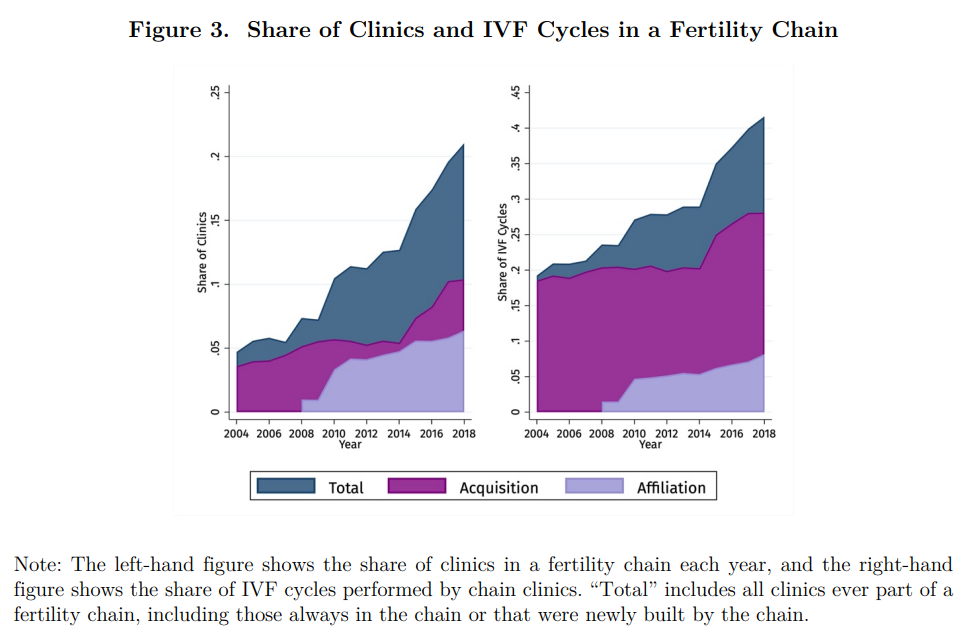
“Most people vilify private equity and the corporatization of healthcare, and rightfully so.” Halle Tecco shared a 2023 study out of Berkley found that private equity actually increases access and improves IVF outcomes by 13.6% after acquisition. Why? The report points to investments in new technologies to build cutting-edge facilities, software, and the sharing of critical information like protocols and best practices. What lessons can we learn from this model to apply in dialysis or value-based kidney care?
Evergreen Nephrology just announced a partnership with Western Nephrology, a nephrology practice with ~30 providers in the metro areas of Denver and Boulder, Colorado. Western is the third nephrology practice in Colorado to partner with Evergreen.
Interwell Health just launched Interwell Learning, a ready-to-use education suite designed to better educate patients about kidney disease and improve outcomes. This offering aligns to the kidney disease education (KDE) reimbursement, so it’s designed for CKD stage 4 and composed of six unique workshops that each include take-home materials, a video, and a one-on-one session with a clinical educator.
Penn State Health has agreed to stop performing kidney transplants for two weeks after scrutiny from federal officials. The health system agreed to stop performing liver transplants in late April while the Organ Procurement and Transplantation Network reviews the program.
Nephrolytics just came out of stealth with its AI assistant, Saya, to bring real-time data analytics, predictive diagnostics, and personalized care plans directly into the hands of nephrologists and healthcare professionals. Meet the team here.
Akili announced its plans to reduce headcount by 46% and evaluate strategic alternatives as it continues its transition away from a prescription-based business model to one focused on subscriptions. The digital therapeutics (DTx) space has seen several players fall victim to challenging market conditions. Better Therapeutics recently disclosed it was laying off its workforce and exploring strategic options, and just one year ago Pear Therapeutics filed for bankruptcy and later sold its assets for around $6 million.
The partnership between the Veteran’s Health Administration and American Kidney Fund will soon be renewed under the management of the VHA Office of Kidney Medicine, according to a recent press release.
A recent study in Health Affairs shows that between 2019 and 2021, remote physiologic monitoring (RPM) via wearables and mobile apps soared by more than 1,300% among Medicaid users. As of March 2023, 34 states had policies on reimbursement for remote physiologic monitoring. Every state except for Vermont billed remote physiologic monitoring claims in 2021, despite the lack of documented policies in some states. (H/t Dr. Sandeep Pulim for flagging this one).
Policy & Regulation
Updates on policies, regulations, and government initiatives.
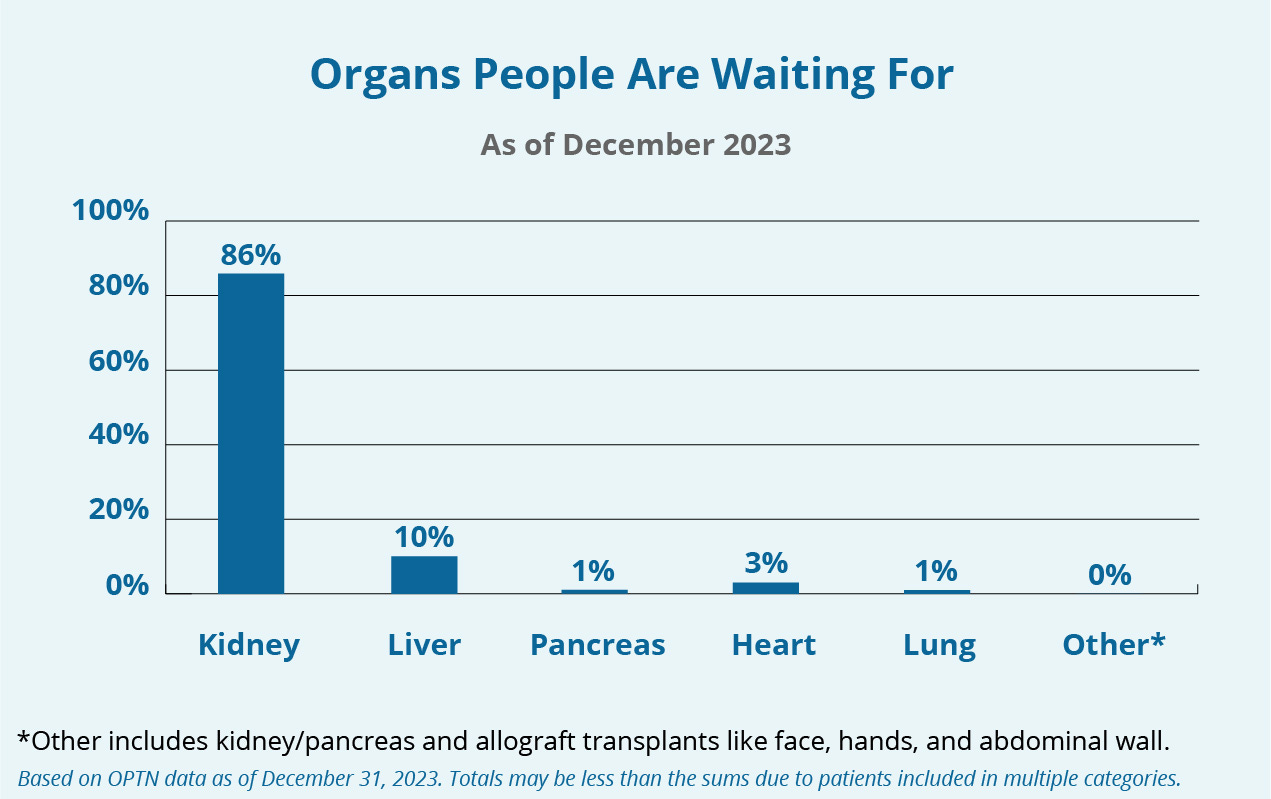
By now you’ve probably seen or heard that CMS announced a new proposed model that aims to increase access, equity, and outcomes in kidney transplantation. The Increasing Organ Transplant Access (IOTA) Model marks an important moment for the transplant community, and complements existing (and future) regulatory efforts for Organ Procurement Organizations, nephrologists, and dialysis facilities to improve the overall transplant system for people with ESRD.
A newly introduced bill would provide funding for staff assistance and more training options for home dialysis. The legislation proposes covering the cost of in-home health care support staff for up to 90 days with an add-on payment to the dialysis payment bundle. (h/t Kerstin Leuther, PhD)
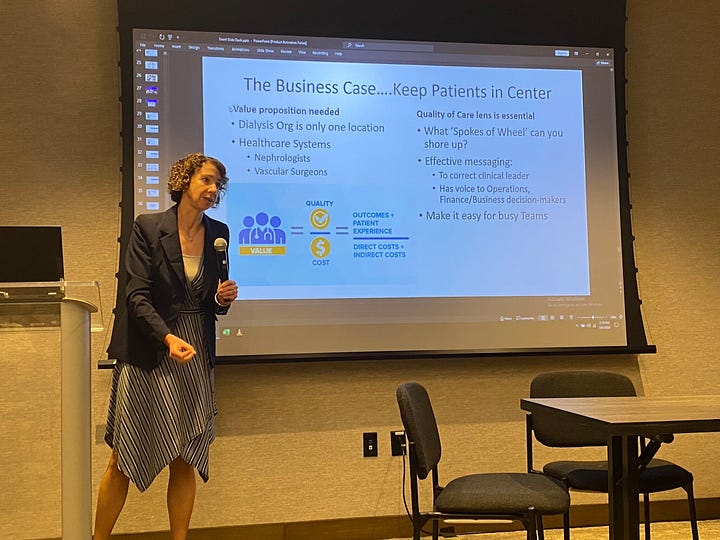
On May 6, 2024, the Kidney Health Initiative (KHI) convened a 50-person vascular access workshop to identify opportunities and challenges for much-needed innovations by exchanging the perspectives of care partners, patients, and clinical care teams with entrepreneurs, companies, investors, National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), and FDA. Below, Dr. Prabir Roy-Chaudhury presents a slide on emerging innovations from Surfacer, DefenCath, InnAVasc, Alio, and CanSim. (H/t to Mark Lim for sharing).



Community Voices
Commentary, opinions, and events across the kidney care community.
Curious why we would need both the End Stage Renal Disease Treatment Choices (ETC) Model and the Increasing Organ Transplant Access (IOTA) Model? Dr. Amber Paulus has us covered. Her recent LinkedIn post shows us why, together, these models ensure comprehensive and balanced incentives across the spectrum of kidney care, avoiding unilateral incentives that could hinder overall progress in patient outcomes.
For those following the latest VBC and CKCC news, a comment thread on Nishant Jalandhara's latest post is an insightful collection of diverse POVs on what's happening in the space. It includes both high-level guiding wisdom and in-the-weeds candor on what it takes to participate in these models.
“With these models, CMMI appears to be trying to answer an important question: Are patients with advanced kidney disease unique enough to require a separate payment model?…”
— Dr. Terry Ketchersid, SVP at Interwell Health
Last month we shared a paper published in Kidney International Reports by Drs. Ben Hippen, George Hart, and Frank Maddux on a proposed transplant-inclusive VBC model, or TIVBC. Dr. Hippen spoke to Nephrology Times about the proposed TIVBC model in a recent interview.
Want to understand 36 Medicare Value-Based Programs in 6 minutes? You know exactly where to look. Dr. Eric Bricker and his whiteboard are back at it with this quick summary of pay-for-performance (P4P), bundled payments, and shared savings models. If you’re like me and feel like you need a refresher on these programs every other week, this one’s for you. PS - he also shared this video on “the secret to primary care profitability” with lessons from Walmart and VillageMD.
Dr. Yubin Park recently shared yet another fascinating data visual, this time illustrating Medicare FFS vs. Medicare Advantage ratios across the United States in 2022. The more left, the more FFS members. The left arrow implies that the county has 100% FFS, and vice versa for the right arrow — 100% MA members. In terms of color, the more red, the more FFS members, while the more blue, the more MA members.
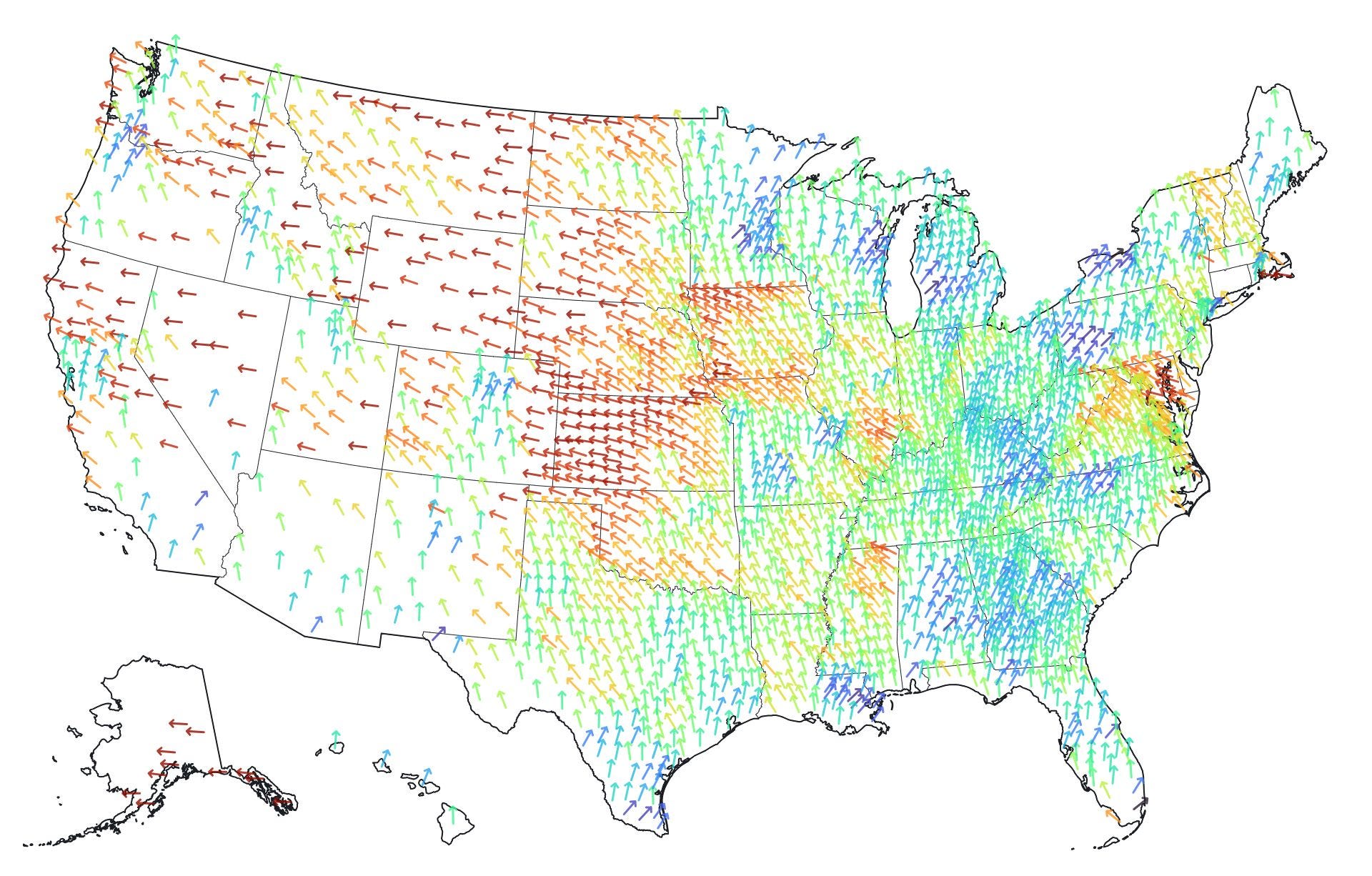
Interactive map via Yubin Park, PhD Bill Hunter, President & CEO at Canary Medical, wrote a fascinating post about the “enshittification” — yes, you read that right — of medical devices and technologies. The term means the gradual degradation of a platform or service, as part of a cycle in which it first offers benefits to users to attract them, then pursues more and more profits at their expense. He makes the case we should be prioritizing innovation to improve commodity device performance, rather than focusing entirely on taking market share at high prices in large markets.
Jeff Parke penned a perspective piece on the opportunity to embed Community Dialysis Advocates (CDAs) into multidiscplinary care teams. He shared his 25-page paper on LinkedIn last week to show how CDAs can serve as a bridge between patients and medical staff, while also increasing empathy, reducing costs, improving outcomes and quality of life.
Matthew Holt wrote a great blog post about all the recent assessments you might have seen floating around about the effectiveness of diabetes care management solutions. He writes, “You can look at virtually any aspect of health care and find ineffective uses of technology that don’t appear to be cost effective, and yet they are widespread and paid for — So why are the knives out for digital health specifically?
An article in MedCity News talks about the polarizing rhetoric around digital health these days (see above). Authors Alyssa Jaffee and Mona Siddiqui, MD, MPH, MSE share thoughts on the early innings for healthtech with examples like NOCD, Jasper Health, GroundGame.Health, Waymark, and Author Health.
“As the number of polychronic Americans rises, the era of a fragmented, point solution digital health ecosystem will fall in favor of a more interconnected and integrated landscape. Consumers, across all aspects of their life, desire solutions that address all their needs.”
— Alyssa Jaffee, 7WireVentures
Renal Research Institute (RRI) and the Karolinska Institutet just announced a joint symposium at the upcoming ERA event in Stockholm next week. The event will be titled "Prevention of CKD progression: the impact of new therapeutics," and focuses on new therapies like GLP-1 and SGLT2i drugs.
In this week’s Signals poll I asked you which of these you consider to be the most trustworthy source of news and insight on your area of healthcare? There’s still time to share your thoughts here. PS - where would you rank industry newsletters like this one if it were an option?
A Closer Look
Here’s a closer look at a few headlines from above and why they matter:
1. The Increasing Organ Transplant Access (IOTA) Model
The Increasing Organ Transplant Access (IOTA) Model marks an important moment for the transplant community, and complements existing (and future) regulatory efforts for Organ Procurement Organizations, nephrologists, and dialysis facilities to improve the overall transplant system for people with ESRD.
Why it matters: The model would run for six years, beginning January 1, 2025, with the aim to:
Increase access to kidney transplants for people living with end-stage renal disease.
Improve the quality of care for people seeking kidney transplants.
Reduce disparities in kidney transplantation.
Increase the efficiency and capability of transplant hospitals selected to participate.
Transplant hospitals assigned to participate in the model would be assessed on how well they increase the number of transplants, improve equity in the transplant process, increase organ acceptance rates, and improve post-transplant outcomes.
2. A New Home Dialysis Bill
The Improving Access to Home Dialysis Act (HR-8075) was introduced on April 18 in the U.S. House of Representatives by Reps. Carol Miller (R-WV), Marilyn Strickland (D-WA), Earl Blumenauer (D-OR), and Mariannette Miller-Meeks (R-IA). This bill aims to increase access to home dialysis by providing trained, professional staff assistance to patients in the home and ensuring that all patients are given the education and support they need to utilize this modality if they so choose.
Why it matters: If passed, the new law would mandate that patients get proper education on all of their dialysis options, expand the universe of healthcare providers who can provide home dialysis training, and cover the costs of in-home healthcare support staff for patients when they are beginning their home dialysis journey.
3. Home as a Health Care Hub
Two weeks ago the FDA announced the launch of a new initiative, Home as a Health Care Hub, to help reimagine the home environment as an integral part of the health care system, with the goal of advancing health equity for all people in the U.S. But here’s the part you may not have on your home health bingo card. The hub will be designed as an Augmented Reality/Virtual Reality (AR/VR)-enabled home prototype, with the $1.2 million project expected to be completed later this year.
Why it matters: FDA has been considering how to ensure the safety of these devices since 2010, when the agency released a white paper on the topic. The Home as a Health Care Hub prototype is the beginning of the conversation—helping device developers consider novel design approaches, aiding providers to consider opportunities to educate patients and extend care options, generating discussions on value-based care paradigms, and opening opportunities to bring clinical trials and other evidence generation processes to underrepresented communities through the home.
Ultimately, lessons from this initiative could inform future regulation in the space and technology used in hospital-at-home programs.
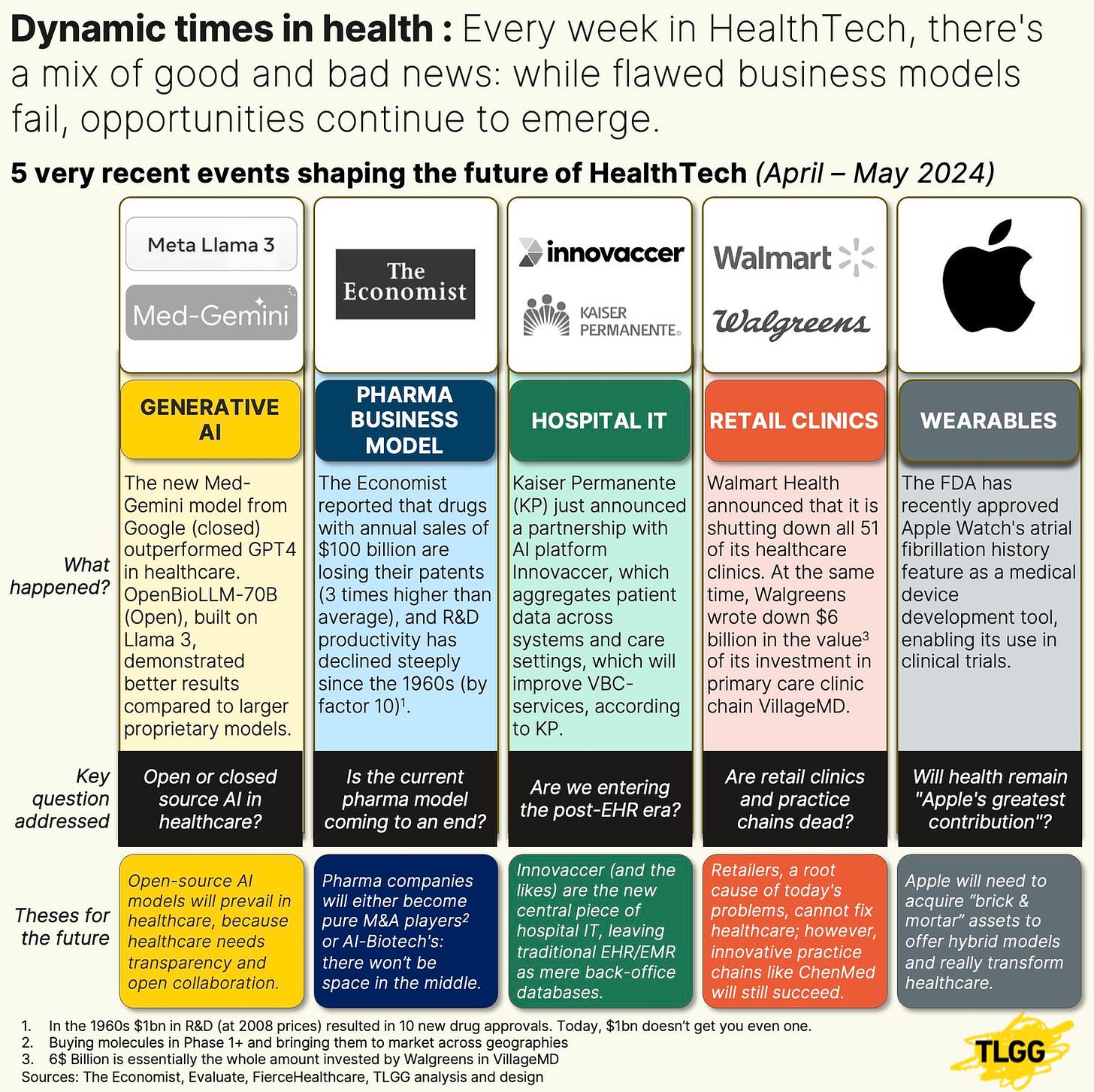
Visuals of the Month
Pictures say a thousand words. What does this one tell us about the impact of big technology and traditional healthcare business models across the Kidneyverse? I always learn something new from Thomas and the TLGG team. This post is one of several thought provoking pieces from the past month.
What do you think, do healthcare technologies hold us back, or catapult us forward?
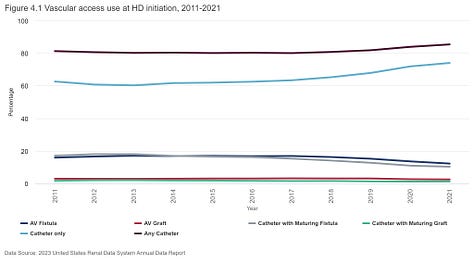
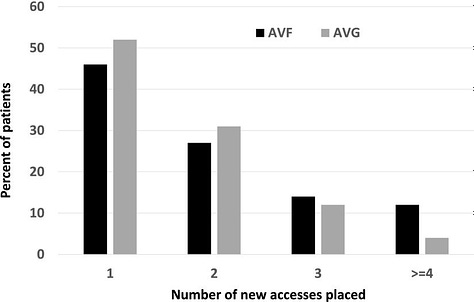
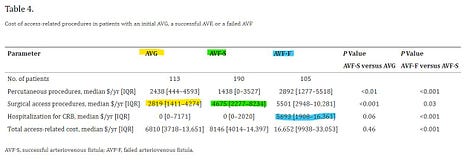
After seeing the KHI vascular access workshop, I spent some time looking at USRDS and recent studies on the economics of access (images below). I’d love to include this one in a broader discussion, so please share your thoughts in the comments or group chat about ways we can make vascular access better, safer, and more…accessible for patients on dialysis.

![Signals From [Space]](https://substackcdn.com/image/fetch/e_trim:10:white/e_trim:10:transparent/h_72,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F2efc1ef1-ba0b-4ca3-b9f6-a9a790da4b38_1344x256.png)