Signals Recap: Ozempic's Latest Approval, EKDA on Reddit, Lilly Stops Relaxin, Beta Bionics IPO, NKF Turns 75, & More...
A collection of news, research, funding & community voices shaping the future of global kidney health
We’re back in action with another Sunday batch of headlines, research, community updates and open roles across the Kidneyverse. Welcome to the 192 new subscribers who joined us last month to shape the future of global kidney health.
If you find this information valuable, please consider sharing this newsletter with 1-2 friends or colleagues. You’ll even earn free access to paid Signals content, including posts, KOL videos, data room, and Slack. Thank you for being here.
In this issue
FDA approves Ozempic to treat kidney disease
Reddit EKDA debate on paying kidney donors
A new milestone in xenotransplantation
Trump’s latest executive orders on healthcare
Health systems pushing for value-based care
Beta Bionics opens the medtech IPO window
NKF turns 75: celebrating top kidney milestones
Should we be talking about cybersecurity more?
Visual: KCC entity spending trends per beneficiary
A new way to treat pain in dialysis patients?
Links between climate and kidney health
Open roles around the Kidneyverse
& more…
Updates
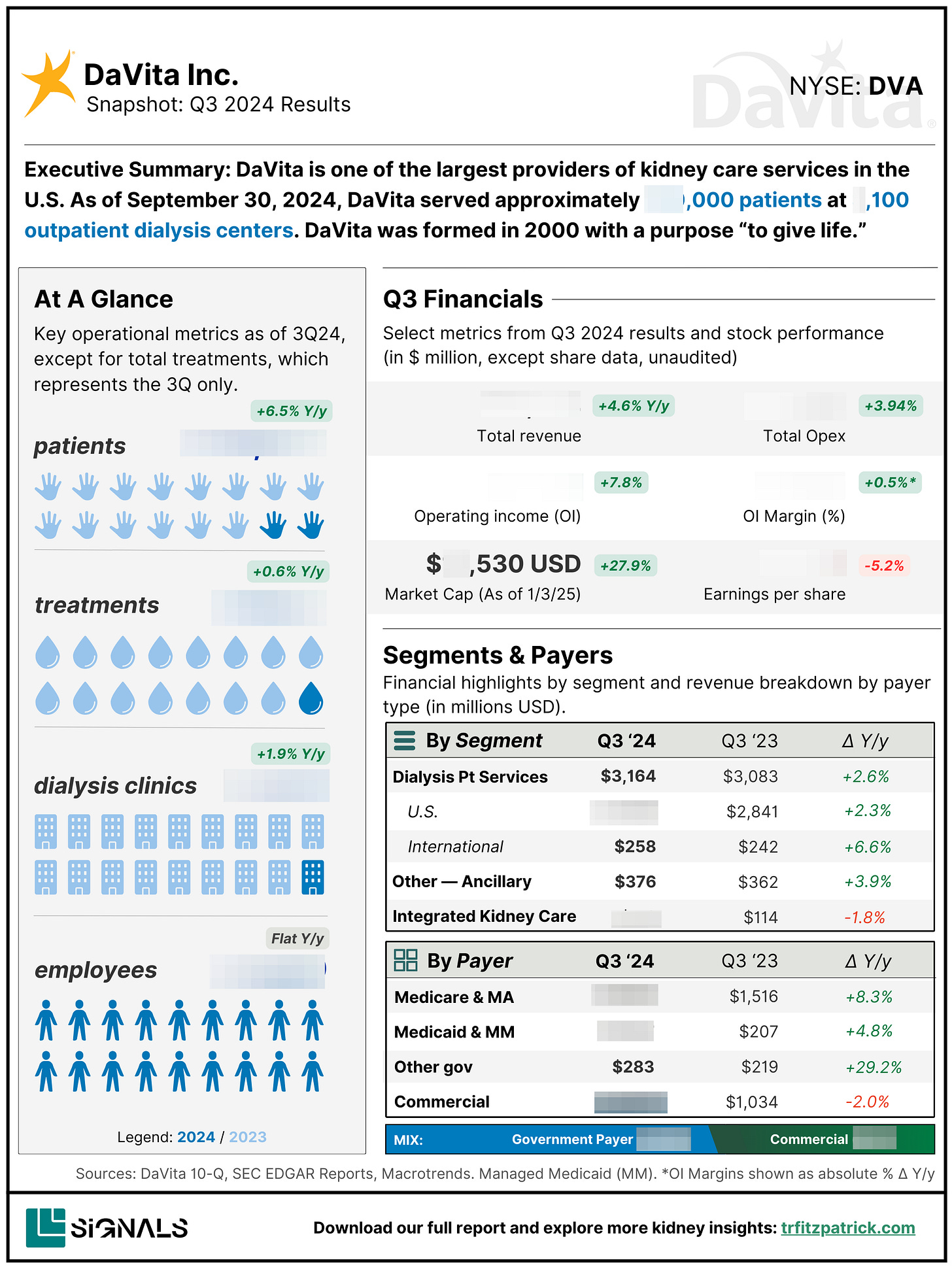
ICYMI: We launched Signals Snapshots to help tell company’s stories. We aim to give you a bird’s-eye view of what companies do, who they serve, how they make money, and what their top priorities and milestones look like. These are designed as practical resources for anyone working in the kidney space—whether you’re building a business, growing a startup, conducting research, or diving into diligence. Have a company in mind you want us to tackle next? Let us know.
We’re also opening up the Slack #general channel so you can join the conversation and see the magic firsthand. I’m loving the back and forth questions, discussions, and candor you just can’t get on social media. People helping people. Paid subscribers get full access to all channels like #transplant, #dialysis, #VBC, #policy, #jobs, #questions and more.
Signals
F.D.A. Approves Ozempic to Treat Kidney Disease
Summary: The FDA has approved Ozempic to reduce the risk of worsening kidney disease, kidney failure, and cardiovascular death in people with both Type 2 diabetes and chronic kidney disease (CKD). In a clinical trial, Ozempic lowered the likelihood of serious complications by 24% compared to a placebo. This decision expands the blockbuster drug’s use beyond diabetes and heart disease, offering new hope for a population with limited treatment options.
Thoughts: This is a major win for the millions managing diabetes and kidney disease worldwide. It reinforces the growing role of GLP-1 drugs beyond diabetes and weight loss, adding to the arsenal alongside SGLT2 inhibitors, which have already reshaped CKD treatment. But access remains a challenge. Demand for GLP-1 drugs already far outstrips supply, and insurance coverage will (continue to) be a key battleground. With Ozempic now selected for Medicare drug price negotiations and oral-only drugs newly included in the dialysis bundle as of January 1, affordability and availability are front and center in kidney care policy discussions.
How will Ozempic’s approval reshape CKD treatment over the next 5 to 10 years? What barriers stand in the way of access for patients? For providers? For payers?
Beta Bionics goes public with upsized $204M IPO
Summary: Beta Bionics (Nasdaq: BBNX) has gone public with an upsized $204M IPO, significantly surpassing its original $114M target. The company, known for its iLet bionic pancreas, has rapidly expanded since its FDA clearance in 2023, with over 10,000 patients now using the system. Proceeds from the IPO will fund the development of a bihormonal iLet system, a new patch pump, and expanded sales and manufacturing. As Beta Bionics enters a competitive $17B insulin pump market, its ability to differentiate from industry giants like Medtronic, Insulet, and Tandem will be key.1
Thoughts: This IPO reinforces the growing investor confidence in medtech after a tough few years. Beta Bionics stands out with its fully automated insulin dosing—removing carb counting and manual corrections—but industry experts still question whether it’s a true "revolution" or an incremental improvement. Its real challenge? Scaling adoption while facing off against well-established competitors. The company’s future likely hinges on how quickly it can expand beyond insulin-only solutions to a bihormonal system, a potential game-changer if executed well.2
How might companies in this space (i.e. Beta, Medtronic, Dexcom) and other diabetes tech leaders bridge the gap between diabetes and kidney care? Is this what a possible future might look like with a wearable artificial kidney?
EKDA: Bold Step or Slippery Slope?
Summary: A heated discussion on r/transplant highlights the End Kidney Deaths Act (EKDA), a proposed bill aiming to prevent up to 100,000 deaths and save $37 billion annually by expanding access to kidney transplants. Supporters argue that EKDA would overhaul outdated policies, prioritize transplants over dialysis, and provide financial incentives for living donors. However, the bill has (understandably) sparked strong emotions, particularly around its funding mechanisms, ethical concerns about incentivizing donation, and skepticism over whether it truly addresses systemic issues in organ allocation and healthcare access. Some worry that the focus on transplants could divert resources from improving dialysis care, while others see it as a long-overdue correction to a system that traps too many patients in expensive, lower-quality care.
Thoughts: As I’ve written before, EKDA is ambitious. The debate here reveals deep fault lines in how we approach kidney care. Supporters argue that prioritizing transplants over dialysis is both clinically and financially sound, but skeptics see a "slippery slope"—worrying that financial incentives could lead to unintended, unequal outcomes. Some contrast the cash incentives with the Michigan bill proposing tax credits and paid leave, questioning whether financial support should take the form of reimbursement rather than a lump sum. Equity is a major concern—who will benefit most, and will it leave lower-income dialysis patients behind? One point that stuck with me: Even if EKDA delivers 10,000 new transplants a year (a huge jump from today’s 300–400), it wouldn’t "end the waitlist” of more than 90,000 people. And what happens if people step forward for the $50K incentive but transplant centers, which are already cautious about living donors, say no? Big questions, high stakes, and a lot to unpack—I’d like to hear what you think.
What do you think about paying donors to donate their kidney to a stranger? What would need to be true for this system to work?
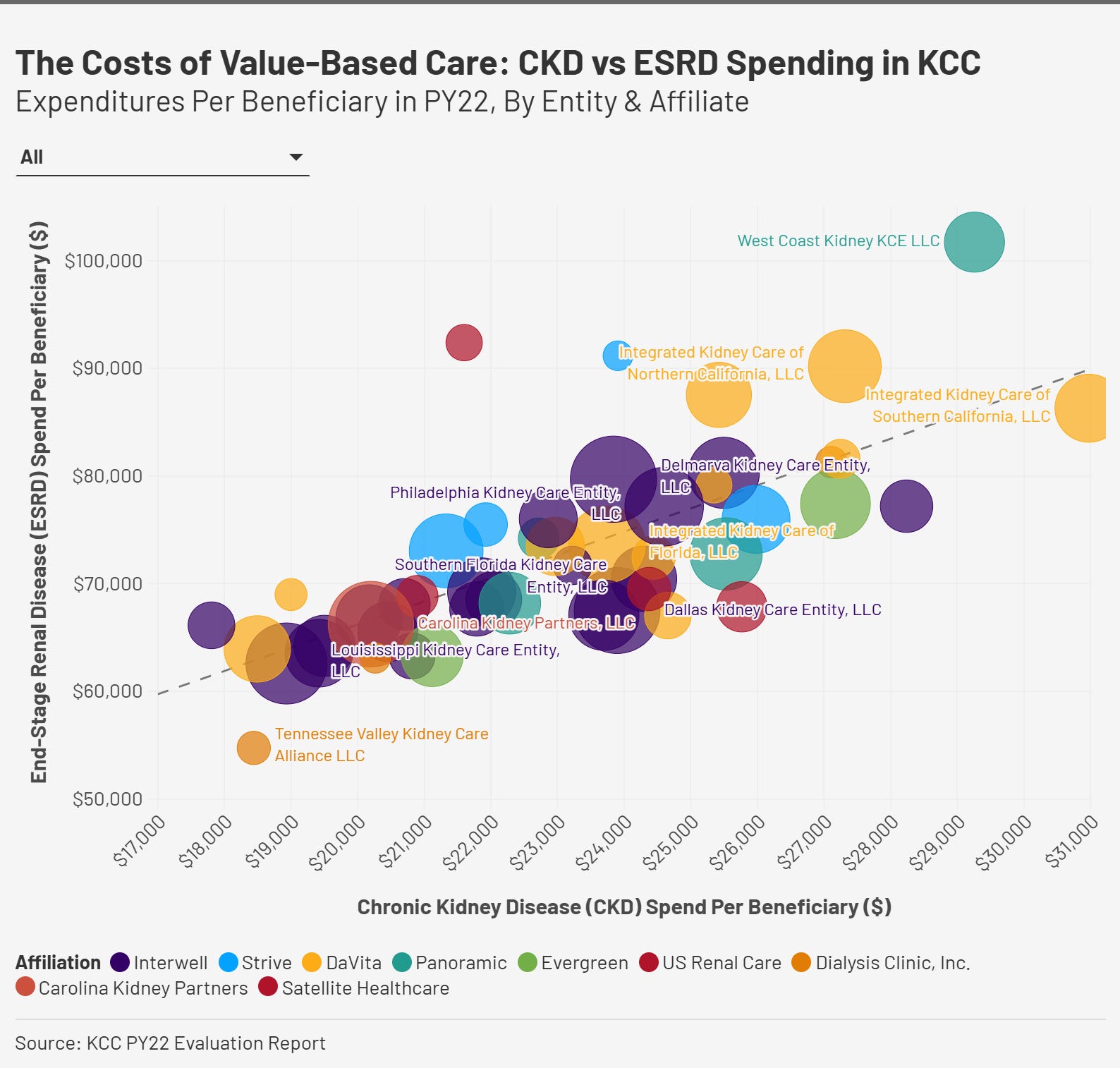
Visual of the Week
Per Beneficiary CKD vs. ESRD Spending. In year one of the Kidney Care Choices (KCC) program, there was a general correlation between higher CKD spending and higher ESRD spending, though some entities managed to contain ESRD costs despite significant CKD expenditures. The scatter plot visualizes this relationship, with CKD spending on the x-axis and ESRD spending on the y-axis. Each bubble represents a participating entity, with larger bubbles indicating those managing more total beneficiaries (CKD + ESRD). The interactive chart shows the specific numbers for each entity.
While most organizations cluster within a moderate spending range, a few stand out as outliers—some spending heavily on CKD but still incurring high ESRD costs, others achieving cost efficiencies with lower-than-expected ESRD spending. Notably, certain affiliations (e.g., Interwell, DaVita, Strive) exhibit distinct spending patterns, suggesting different care management strategies. As KCC enters its fourth year, these early trends will be key to understanding how investments in CKD care translate to long-term ESRD cost containment. See the CMS findings at a glance here.
News

F.D.A. Approves Ozempic to Treat Kidney Disease [WSJ] [Novo PR]
Trump’s initial orders reverse Biden on health care costs, protections from discrimination [STAT]
NBA Hall of Famer Dwyane Wade reveals cancer diagnosis and partial kidney removal [NBC]
Recipient of pig kidney transplant reaches a milestone [NPR] (H/t for sharing Sen. Bill Frist)
How the NHS is reducing kidney failure risk nationally [NHE]
Health systems ditch incrementalism in value-based care [Becker’s Review]
Inside the lab that’s the beating heart of Medtronic’s product pipeline [Star Tribune]
Lilly Cuts Mid-stage Relaxin Study in Chronic Kidney Disease for ‘Lack of Foreseeable Clinical Benefit’ [BioSpace]
Proton’s device aims to help those with kidney disease and cut heart-failure risks [TechCrunch] (H/t Rory St Clair)
Research
Effects of statins on kidney function in older adults [JAGS]
Risk-directed management of chronic kidney disease [Nature]
Safety of Kidney Transplantation from Donors with HIV [NEJM] [U Miami]
Behavioral intervention decreases how much pain affects daily activities in people with dialysis-dependent kidney failure [NIH]
Enhancing gene transfer to renal tubules and podocytes by context-dependent selection of AAV capsids [Nature]
Urology on a changing planet: links between climate change and urological disease [Nature]
Renal dysfunction contributes to deteriorated survival outcomes in patients with upper and lower gastrointestinal bleeding: insights from a cohort study of 1160 cases [Scientific Reports]
Community
Anniversary: National Kidney Foundation’s 75th Anniversary: Top Milestones That Changed Kidney Care [NKF]
Thread: Help save up to 100,000 lives & $37 billion in taxes with the End Kidney Deaths Act [Reddit]
Podcast: Abe Sutton hosted Jennifer Erickson on the Rubicon Founders podcast in September to talk organ reform, OPO leadership, and transparency. [Spotify]
Drug Duopolies: Everywhere you look in biopharma, you see drug duopolies. But why is this such a common structure? [Sleuth]
Sonavex and Prisma Health just announced the first patient has enrolled in the MAFASA trial. [Sonavex] (H/t to John Rappe for sharing)
Delta4 Secures European Patents for Two Compounds as Candidate Treatments for Focal Segmental Glomerulosclerosis (FSGS) [BioSpace] (H/t Kurt Herpel)
Security: Why is healthcare so bad at cybersecurity? [Second Opinion]
Many die awaiting kidney transplants in Wisconsin, so this man donated his [Wisconsin Watch]
Report: 2024 year-end market overview: Davids and Goliaths [Rock Health]
Report: Digital Health Trends 2024: Implications for Research & Patient Care [IQVIA]
Jobs
Director, Provider Partnerships at Monogram Health
Transplant - Hepatology at Piedmont Transplant Institute
Exec Dir, Product Strategy Lead at Novartis
Assoc Dir, Patient Advocacy at American Kidney Fund
Director, US Marketing - Nephrology at Alexion
Assoc Dir, Innovation PM at AstraZeneca
Director of Strategic Sales at Interwell Health
Head of Clinical Outcomes at DeLorean AI
Chief of Staff at Somatus
Made Possible By
Signals is made possible with the generous support of our sponsors. We are grateful to partner with organizations committed to advancing kidney care and innovation. This post was made possible by Roivios and 3ive Labs. Thanks team!
Castellanos LE, Balliro CA, Sherwood JS, Jafri R, Hillard MA, Greaux E, Selagamsetty R, Zheng H, El-Khatib FH, Damiano ER, Russell SJ. Performance of the Insulin-Only iLet Bionic Pancreas and the Bihormonal iLet Using Dasiglucagon in Adults With Type 1 Diabetes in a Home-Use Setting. Diabetes Care. 2021 Jun;44(6):e118-e120. doi: 10.2337/dc20-1086. Epub 2021 Apr 27. PMID: 33906916; PMCID: PMC8247518.
I’m a BU grad, so I was proud to learn the iLet was invented in the lab of Ed Damiano, a BU College of Engineering research professor of biomedical engineering who cofounded Beta Bionics as a public benefit corporation back in 2015. He first began work on the device in 2002—inspired by his infant son’s battle with diabetes. This is a great story about Ed’s work and what the company stands for.

![Signals From [Space]](https://substackcdn.com/image/fetch/e_trim:10:white/e_trim:10:transparent/h_72,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F4d588ac1-7fac-4bd4-829d-fc7b4e8f1326_1512x288.png)

![Signals From [Space]](https://substackcdn.com/image/fetch/w_36,h_36,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F55686857-6b99-45a6-ac0f-09c9f023f2a0_500x500.png)




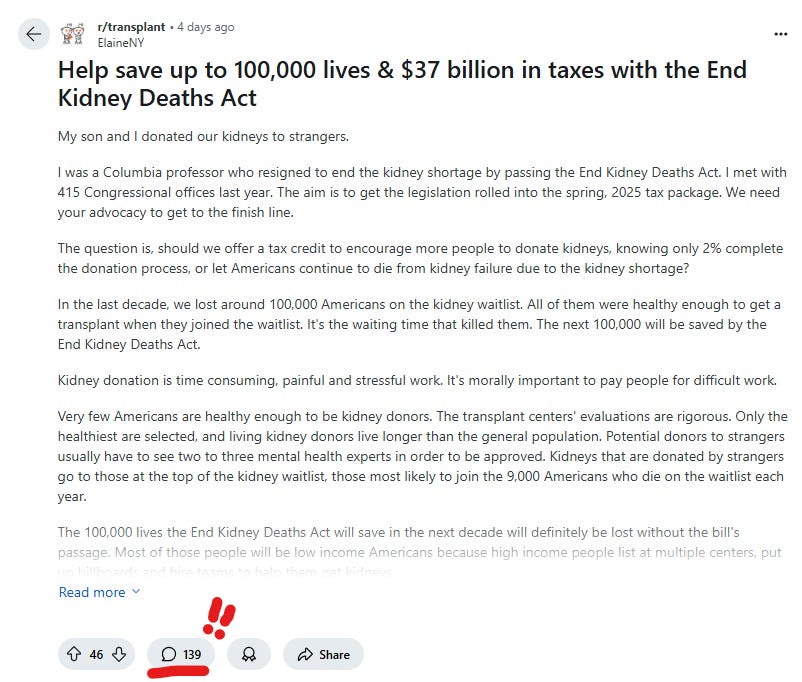
It appears obvious that we need to utilize different approaches as our current system is failing so many, resulting in needless suffering and death of thousands. This pilot program will evaluate the effectiveness, as well as reveal the problems, with providing incentives. This may be an ethical approach needed to address the critical kidney shortage.
To clarify (as Nancy mentioned), this is a pilot and if successful for non-directed donors, could be expanded to all living kidney donors (and would potentially increase the number of people receiving transplants). As a living kidney donor and nephrology nurse, I think it is a disgrace that donors currently PAY to donate kidneys through the expenses of travel, time off work, etc. Let the pilot begin and let's discover the actual outcomes before criticizing this payment method (to encourage more living donors.) And why is it okay to let thousands of people die each year on the transplant waiting list by doing nothing to incentivize donors? Our current system is failing and it is time for a new, bold action like the EKDA. No one intervention is going to fix our kidney crisis, so let's try out many optimization approaches and then determine the best ones that have the most positive impact. Preventing and getting people off dialysis by helping them receive a living donor transplant (and paying donors) will save money, so why not start there?