We should probably talk about (barriers to) home dialysis
How the IM-HOME study reshapes our approach to patient, care partner, and provider-facing barriers to home dialysis.
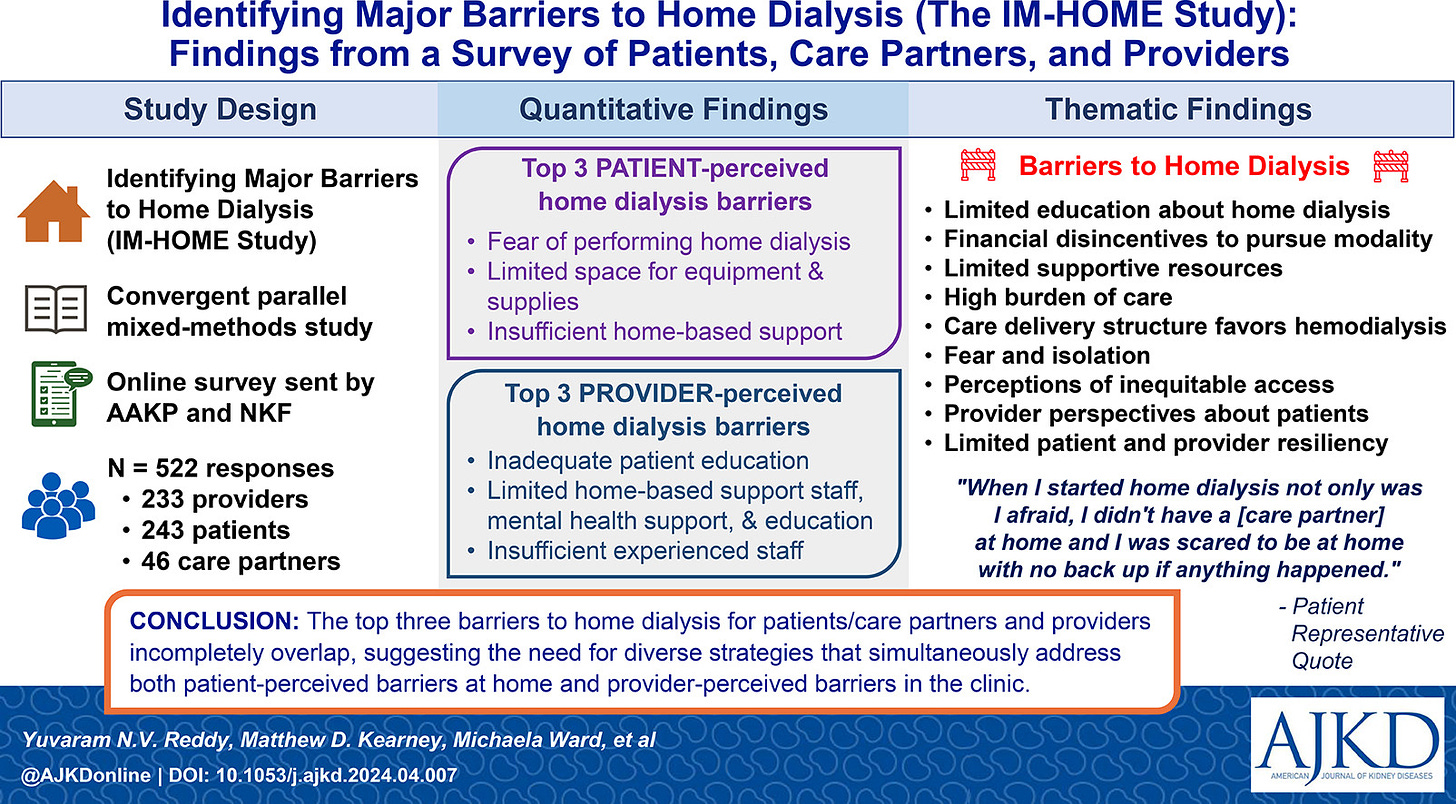
A recent study published in the American Journal of Kidney Diseases provides the backdrop for today’s discussion. Researchers explored barriers to home dialysis as perceived by patients, caregivers, and providers. The IM-HOME study, led by PI Dr. Yuvaram Reddy and colleagues, surveyed a group of 522 participants, including 233 providers, 243 patients, and 46 care partners. Let’s review what we learned from the findings — and what I hope we as a community will do about it.1
Truth be told, you’ve likely seen or heard these barriers before. Many past papers and studies have identified them— I’ve co-authored a few in recent years. But what I find most compelling about this particular work is how it ends. After the authors finish weaving together these unique perspectives, they go on to provide a list of clear, actionable next steps toward addressing these gaps in care. And it just so happens these suggested next steps align with recent policy recommendations gaining steam in Washington. More on that later.
For now, let’s use this spark to re-light an open discussion about moving dialysis home, starting with how patients decide to go home in the first place.
The Home Dialysis Patient Journey
No two patient journeys are the same. As much time as we spend talking about how big of a problem kidney disease is in this country, and for good reason, the reality is our current built-for-scale kidney care system misses the trees for the forest. Doing a complex, live-sustaining treatment “on your own'“ at home is scary.
So, how does someone get from “I need dialysis” to “I can do dialysis at home”?
The conceptual model below depicts the ideal patient journey to home dialysis. In the upper section (A) of the model, patients—e.g., people with chronic kidney disease stages 3-5, or people receiving in-center hemodialysis—move through 5 distinct phases of home dialysis: (a) referral, (b) education, (c) training, (d) initiation, and (e) maintenance.
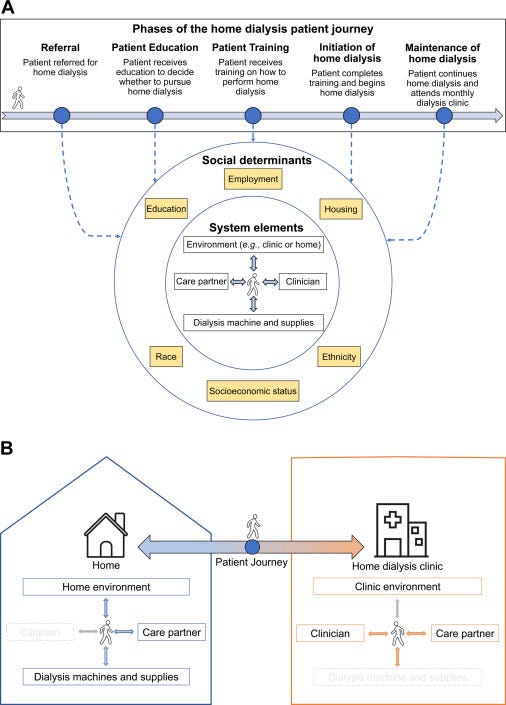
At each of these 5 phases (blue circle), patients interact with 4 system elements (white boxes): providers, care partners, the dialysis machine and supplies, and the environment (e.g., the patient’s home, the home dialysis clinic, and the primary care clinic)—all of which can serve as barriers or facilitators to home dialysis use.
Social determinants (yellow boxes; e.g., education) modify the influence of system elements on the provision of home dialysis.
You’ll notice how the lower section (B) of the model shows a patient receiving home dialysis in two environments: 1) when they are at home performing dialysis, and 2) when they come to clinic for education, training, or monthly physician visits. Within each environment, arrows represent interactions between patients and system elements (e.g., interactions between patients and care partners).
With this model in mind, let’s talk about the survey’s findings.
Top Barriers
The primary outcome for this study was the top three perceived barriers to home dialysis for each of these stakeholder groups (i.e. patient, care partner, provider). They found the top 3 barriers cited by patients and caregivers included fear of performing dialysis at home, lack of space, and the need for home-based support. On the other hand, providers identified poor patient education, limited support staff, and lack of experienced staff as the primary obstacles.
"When I started home dialysis, not only was I afraid; I didn't have a care partner at home and I was scared to be at home with no backup if anything happened."
Study Insights
The study delved deeply into the experiences of patients, caregivers, and providers, revealing nine themes that paint a complex picture of home dialysis. Six of these themes matched expectations: limited education, financial disincentives, lack of resources, high burden of care, a built environment favoring in-center dialysis, and fear of isolation. But the study also surfaced three new themes: inequities in access to home dialysis, provider perceptions that underestimate patient capabilities, and the importance of resiliency.
Patient stories bring these challenges to life. One patient shared, "When I started home dialysis, not only was I afraid; I didn't have a care partner at home and I was scared to be at home with no backup if anything happened." Another echoed this, highlighting the lack of medical support at home as a major worry. A care partner emphasized the complexity of chronic kidney disease (CKD), saying that patients need a lot of education and support to feel confident managing dialysis at home.
Providers had their own concerns. A nurse practitioner pointed out that home dialysis is often offered as a last resort, not the first best option, and patients aren't always told about the time commitment involved. A nephrology nurse criticized the lack of early education for CKD patients, explaining that many are too sick to make informed decisions by the time they start dialysis. This gap in early education, along with financial barriers, pushes many towards in-center hemodialysis.
"Home dialysis is often offered after a failure [of] in-center hemodialysis […] making it appear to be a last ditch try instead of the first best option. Also, providers that say they encourage [home dialysis] aren't honest about [the] process[.] [They] make it sound very easy with little time commitment and it isn't.” —Nurse Practitioner
The emotional toll of dialysis also came through clearly. One patient described their fear and isolation, saying that a nurse's strong push for in-center dialysis left them feeling hopeless and considering skipping treatment altogether. These personal stories highlight the urgent need for a more patient-centered approach, where education, support, and encouragement are front and center for those considering home dialysis.
Two promising strategies worth exploring are (i) assisted home dialysis and (ii) peer support. Assisted home dialysis, involving temporary or permanent help from care partners or hired staff, can reduce patient fear, provide necessary home support, and improve education. Peer support, where trained patients provide social and educational support to peers, can also alleviate fears, enhance patient education, and offer additional support for clinic staff. Currently, Medicare does not pay for assisted home dialysis; however, recent data suggest it is feasible, safe, and possibly effective in improving home use. We have written about the need to validate peer support for kidney failure in the past.
Why It Matters
In a nutshell, the study's insights underscore the need for a more tailored, empathetic, and comprehensive approach to home dialysis. One that addresses both the personal and systemic hurdles faced by patients and providers alike.
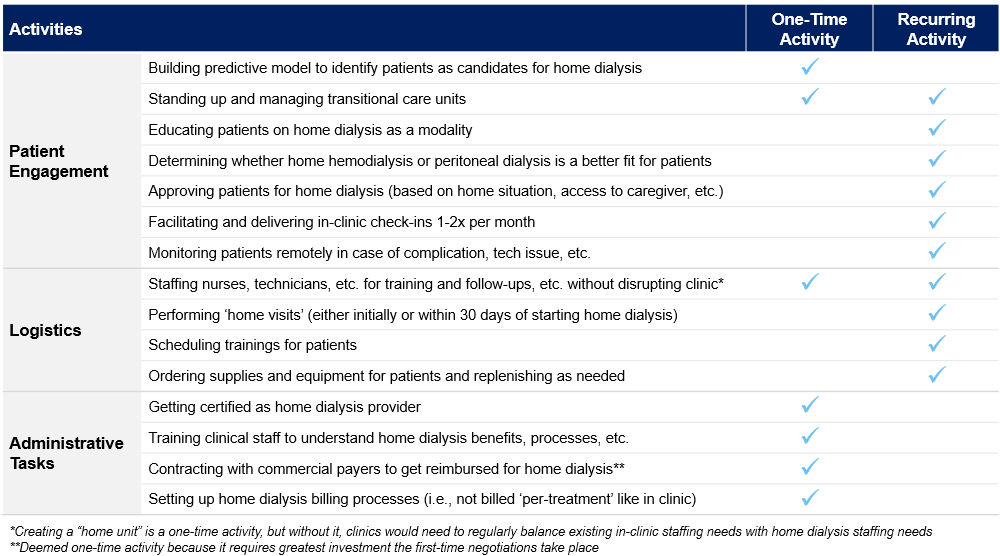
For example, current obstacles to home dialysis often stem from financial and operational constraints within the dialysis system. This focus means that while home dialysis can offer significant benefits, it also faces considerable barriers, such as “home unit” logistics and a lack of professional home support, which remains an ongoing hot button issue in the industry.2
Recommended solutions to these barriers include improving education for both patients and providers, reforming reimbursement policies, and investing in support structures that can facilitate home dialysis. By tackling these challenges, we can create a more patient-centered approach that encourages home dialysis and leverages its potential to improve quality of life for those with chronic kidney disease. The key is to balance the broad, population-level focus of current kidney care systems with the unique, individual journeys of home dialysis patients.
These insights underscore the urgent need for policy changes and innovative solutions to make home dialysis more accessible and effective, highlighting the ongoing discussions in the industry about the best ways to support this vital treatment option.
Resources & Data
Ready to keep exploring this topic? Below are several resources worth exploring to expand your breadth and depth of knowledge, and the data to support them.
Starting the dialysis conversation:
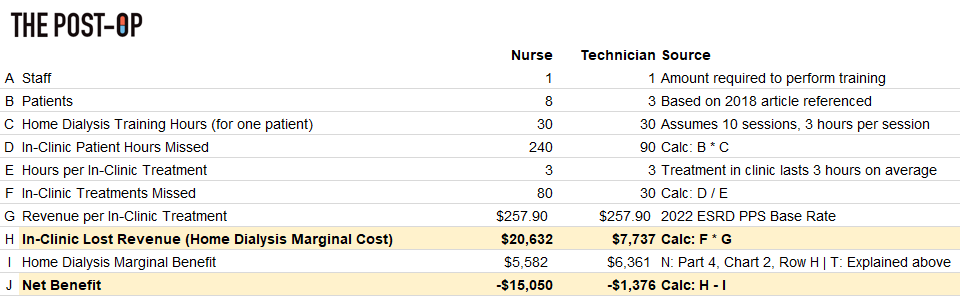
wrote an incredible 7-Part series on the business of kidney care in the United States. Part 4 unpacks the operations, clinical, and business considerations of home dialysis before Part 5, which goes deeper into how we can increase that 14%. This is a must-read if you work in clinic operations, value-based care, or, frankly, anywhere in CKD or ESKD.
Home Dialysis Bill: In April we wrote about the home dialysis bill that would provide funding for staff assistance, plus more training options for home dialysis. The Improving Access to Home Dialysis Act (HR-8075) was introduced on April 18 in the U.S. House of Representatives. If passed, the law will mandate that patients get proper education on all of their dialysis options, expand the universe of healthcare providers who can provide home dialysis training, and cover the costs of in-home staff support when they’re beginning that critical phase of their journeys.3
USRDS Home Dialysis: The most recent Annual Data Report includes a section on Home Dialysis in adults. Bookmark this ADR if you work in this space — it is the closest thing to a benchmark we have available when comparing outcomes across providers and care models.
VR Education & Training: Full disclosure, my day job focuses on solving many of the challenges described in this article. At IKONA, we believe many of these obstacles can be overcome by leveraging the power of immersive technologies like virtual and augmented reality to deliver effective, consistent, on-demand education and training experiences for patients and frontline staff. No surprises here, but we have written extensively about these opportunities. We have also announced several industry partnerships that aim to tackle home dialysis barriers with the likes of Balboa, Fresenius, and Lifeliqe.
Discussion
Home dialysis is a complex topic. We need to better understand each other’s lived experiences, beliefs, strategies, and lessons from helping patients along this journey. Please leave a comment below to let us know what you think about these barriers and key opportunities, or send me a private note directly here.
Thank you for being here. I’d love to hear from you below if you have thoughts on staff-assisted home dialysis or peer support programs for home dialysis.
Keep exploring,
— Tim
Want to support my work?
H.R.8075 - Improving Access to Home Dialysis Act of 2024 — Congress.gov
![Signals From [Space]](https://substackcdn.com/image/fetch/w_80,h_80,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F55686857-6b99-45a6-ac0f-09c9f023f2a0_500x500.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/e_trim:10:white/e_trim:10:transparent/h_72,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F4d588ac1-7fac-4bd4-829d-fc7b4e8f1326_1512x288.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/w_36,h_36,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F55686857-6b99-45a6-ac0f-09c9f023f2a0_500x500.png)



Excellent and insightful review of the IM-HOME article.
I'm the grateful recipient of a preemptive kidney txp from a living donor. What struck me in reading your piece is that the same barriers to home dialysis (save for space at home) are barriers to living donation transplant: fear, lack of education, concern with resources, payment systems, provider perspectives in evaluation, etc. I teach a course at my transplant center on "How to Find a Living Donor" and have encounter these same concerns in almost all patients - in part because the entire transplant structure is designed for decreased donation although living donation is clearly the best treatment. I am new to this space and wonder if you have written previously about living donation or if your company does VR education regarding living donation.
Tim as usual this is an incredible piece of work including the resources we need to stay up to speed (get up to speed) with you and the immensely complex issues and factors in kidney care writ large and with home care in specific.
My bias and point of departure being the overlap of the Venn diagram of:
*Home care (specifically aging in place, management of multiple chronic conditions and well-care)
*Care coordination leveraging AI and remote tech HealthTech platforms for families, patients, caregivers (formal and informal), clinical teams
Home dialysis cuts a wide swath across this overlap.
The accelerant of aging of Americans into Medicare and the CMS mandate around VBC helps to create what I call a “burning platform” that is illuminating the way for real innovation and meaningful changes.
The bill you mentioned is evidence that the CMS and congress sees the handwriting on the wall.
Home care is less expensive. Let’s be honest. One driver is economic.
The incumbent players are excited about this and yes it also holds to their espoused company values of making life with Dialysis more bearable and to improve the quality of life.
Not questioning that for a second.
The industry skews to an older demographic and also to one with multiple chronic conditions.
See above Venn diagram and meta forces colliding.
As a member of a family with a loved one in Dialysis and now home dialysis, I have been deeply in the trenches.
To the frustration of the provider I think too, because I /we have been calling out these nine themes and more, but see little progress.
This in spite of valiant clinic staff, HQ systems people, product and tech people at the machine and supplies company, and under-resourced, under trained staff, overwhelmed nephrologists who know too little about the nuances of this modality, and -and here it is- largely terrified, very sick, disempowered and timid patients.
Many /most of whom do not have strong, informed, present advocates.
What I’m coming to, is that our frustrating and exhausting and frankly medically poor experience is of a family with full access, premier medical providers, resources for additional caregivers, three sibs and spouses local to help, and lots of offline medical advice and expertise to hold the care team accountable.
And yet, it is still a mess, from a care coordination standpoint, from an operations standpoint and from a patient experience.
We have family conversations about what must be happening to patients without strong advocates, or resources. It’s heartbreaking to think about.
Medicaid can’t pull this off in this current state of affairs. And this is a serious #access issue that may create so many failures that the whole concept of home Dialysis -which is a great one- may be invalidated or set back.
The providers are too far over their skis.
The result of not truly understanding the patient experience and journey, is that the providers don’t yet at a corporate level seem to understand what we in software and services call the “unit economics” since this whole sub-industry came into being in the context of fee-for-service and on top of that in the severe chronic category (at scale) of older patients with multiple chronic conditions cascading from diabetes to CKD and ESRD.
It’s a whole delivery system and concept built from best guesses and assumptions and reactive small fixes. It’s been allowed to persist because these unit economics have been masked in fuzzy fee for service bundles and unlimited codes for “the small stuff” to just get things done, masking the messiness of the system.
One suggestion is more and better training and education. @IKONA is a shining example of how an incremental improvement in that single factor has immense benefit and high leverage/impact.
And (not but) it is a kind of spot or point solve that masks a larger picture of an industry trying to extend existing skills and expertise beyond its DNA in terms of service model, unit economics, staffing and staff expertise, modalities of care and state of the actual tech (which, while amazing, is not yet at a “consumer” management state.
Thus the mismatch at the leadership level is unrecognized, and the issues are pushed down to the clinic staff level in this “new” model.
Because there is still so much chaos and so little resourcing at the clinic level, these issues cascade onto the patient and family (if there is one present).
The whole thing collapses when no ongoing resources are present for the patient.
And yet. We know viscerally that home care is more effective in all of healthcare when appropriate) and that “on paper”’it should be a net net benefit for the wellbeing of the patient, a money saver for the payer (mostly CMS), a substantial expansion of business in scalable new sector for providers (just ask my Private equity friends and public company analysts).
But because most of the elderly patients and their families (If they have any /present) are largely unempowered, very sick, dealing with other chronic conditions, the real disconnects have not made their way up the chain.
Sure there are many success stories.
The failures are hidden and largely undocumented.
Nobody wants to dare challenge an insanely stressful and dire situation for fear that they will be “fired” from home dialysis by frustrated providers who are frustrated themselves at the clinic level, and nephrologists who as a group typically outsource the nitty gritty of dialysis detail to centers.
How can we take this data and make real change?
Be more honest about how “beta” home dialysis is now, and ask the provider community to over-resource training at the clinic staff level and ongoing at the patient level, supplies operations, and back office systems from the manufacturer level.
(I asked bluntly one manufacturer (a large public company) and the VP said offline that they are rushing these to market so fast that user interface, training and call center user support are being left to the last thing.. only when things endanger patients does attention go to any kind of improvement. They can already sell all they can make without any improvements).
My bias again being care coordination in this context, I believe that the best hope is with the VBC mandate, more funding earmarked for visiting caregivers /coaches and more *ongoing* education like what your team does, and a more empowered and vocal boomer and gen x population shocking the old line incumbents into better accountability.
In the end this is a consumer self-managed service.
That’s not easy.
That’s a new concept to healthcare.
And certainly new to kidney care incumbents across the value chain.
There will be some uncomfortable growth, but it is healthy.
Count me #optimistic
Keep up the great work!