This Year in Kidney Polls: 2024 Edition
A look back at what we heard and learned from the community through our weekly polls, trivia, and group discussions
Last December, I set a daily calendar reminder to help keep my LinkedIn posting consistent: polls at the start of the week, deep dives mid-week, and personal stories to wrap things up.
What I quickly learned was that the polls set the tone for the entire week. They plant the seed for deeper conversations and stories that follow. While I write a lot more than what you see here in the newsletter or on LinkedIn, I use a "barbell strategy" — long-form, data-driven analysis on Substack and shorter, story-driven engagement on LinkedIn. Most of you discover my writing through LinkedIn and then dive deeper into Substack.
On any given month, I have anywhere from 5 to 50 drafts in progress. As they move closer to being published, I start thinking about how I’ll engage readers through polls. Whether it’s a ‘Fill in the Blank’ or a ‘Magic Wand’ scenario, the goal is always the same: spark thought, conversation, and engagement on the unique opportunities and challenges in kidney health.
Today, let's revisit a few of those polls to uncover key insights and lessons from the community that might shape how we think about kidney health in 2025.
Poll Topics
General
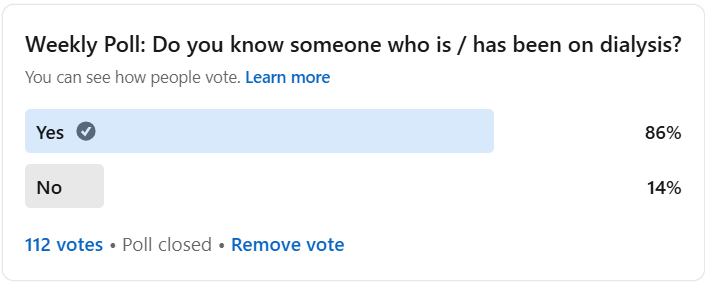
1. Do you know someone who is or has been on dialysis?
Summary: 86% of respondents know someone who has either been on dialysis or is currently on it. This highlights how common kidney disease is, especially within communities already engaged with kidney health. [Link to poll here.]
Thoughts: This poll highlights the widespread nature of kidney disease, which affects nearly 1 billion people globally. The fact that so many of us are connected to someone who has experienced kidney failure reinforces the urgency for better prevention, treatment options, and increased awareness. I often wonder: if more people knew what dialysis was really like— a modern Shep Glazer moment— how might that influence (or galvanize) the court of public opinion?1
Lately, I’ve also been reflecting on how we capture and amplify our collective voices. There are two main ways to make our voices heard: shout louder (grow influence) or add more voices (grow readers). In the true spirit of Signals, let’s not only continue raising awareness within this community but also extend it beyond. By connecting more people to this conversation, we can push for the change needed to improve care, treatment, and prevention.
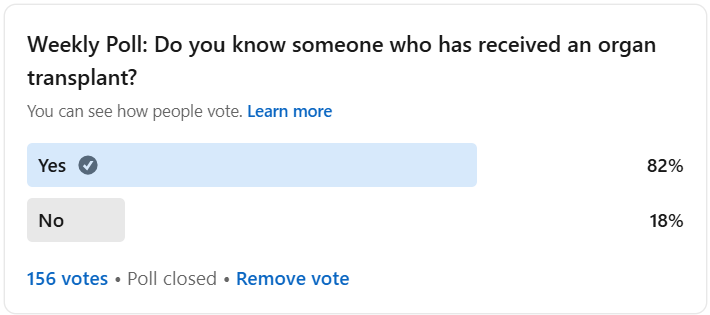
2. Do you know someone who has received a transplant?
Summary: An overwhelming 82% of respondents indicated that they know someone who has received an organ transplant. This highlights the growing visibility of transplantation and its role in medicine, as well as the impact it has on people’s lives. It’s clear that organ transplants, while still a complex medical process, are becoming more familiar to many. In the United States, we reached the one millionth organ transplant mark in 2022. At the time, there were around 400,000 people living with a functioning transplant. [Link to poll here.]
Thoughts: While the majority of people in this poll are connected to someone who has had a transplant, it's important to recognize the barriers that still exist for many patients. Imagine needing an organ and joining the 113,600 people on the waiting list, only to face a 50% chance of receiving that organ within the next five years. This statistic underscores the urgency of expanding access to transplantation, as well as the challenges faced by patients who are waiting for a life-saving procedure.
The economic impact of increasing organ donations is also hard to ignore. Taxpayers could save $40 billion in 10 years if more organs were recovered. Without a transplant, patients with kidney failure are reliant on costly and painful dialysis, which costs Medicare $36 billion annually—more than the annual budget for NASA and the CDC combined.
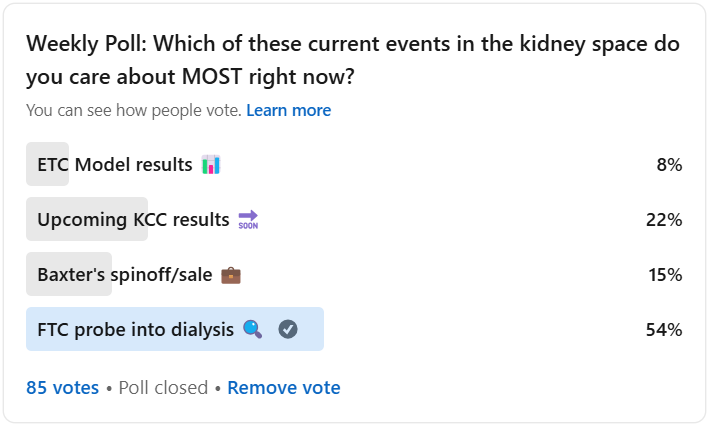
3. Which of these current events in the kidney space do you care about MOST right now?
Summary: In response to the question of which current kidney care event people care about most, 54% of respondents chose the FTC’s probe into dialysis, followed by the upcoming Kidney Care Choices (KCC) results at 22%. Baxter's spinoff and the ETC Model results garnered 15% and 8% of the vote, respectively. [Link to poll here.]
Thoughts: The FTC probe remains top of mind for many, reflecting concerns over anti-competitive practices in the dialysis industry. With Fresenius and DaVita under scrutiny, this investigation has the potential to reshape how dialysis care is delivered. Since the poll, we’ve learned about the early KCC results (PY1) and Baxter's decision to sell their kidney care business to Carlyle Group, which highlights shifting uncertainty and public market dynamics. As for the incoming administration's impact on the FTC's investigation, while recent nominations suggest merger review will return to traditional consumer welfare principles, aggressive antitrust enforcement is unlikely to disappear entirely—especially in light of the populist approach that defined the first Trump administration. These events show how the future of kidney care is deeply influenced by economic, political, and regulatory forces.
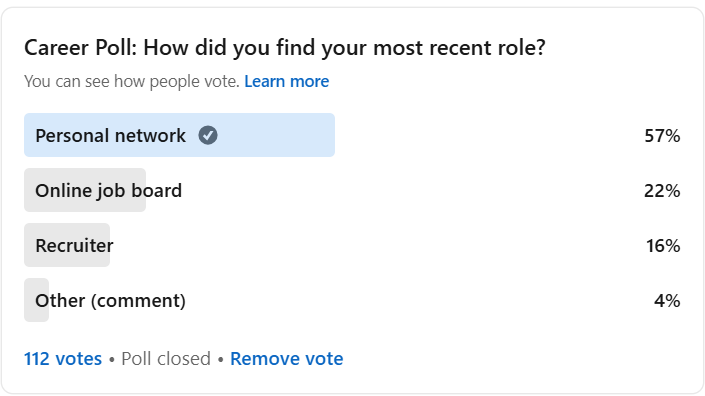
4. How did you find your most recent role in the Kidneyverse?
Summary: The majority of respondents (57%) indicated that they found their most recent role in health tech through their personal network. This highlights the ongoing importance of relationships and networking in career advancement within the Kidney-verse. Online job boards (22%) and recruiters (16%) were secondary options, but still played notable roles in helping people land jobs. [Link to poll here.]
Thoughts: Your network remains one of the most powerful tools for finding new opportunities. In our corner of the healthcare + technology Venn diagram, where the ecosystem is relatively smaller and highly specialized, personal connections seem to be more important than ever. This reinforces the idea that building and maintaining strong professional relationships can open doors to new roles. I’m excited to think about how we can facilitate even more of these connections. Stay tuned for updates as we work to create an even stronger platform for job seekers and employers in kidney health and beyond.
Perspectives
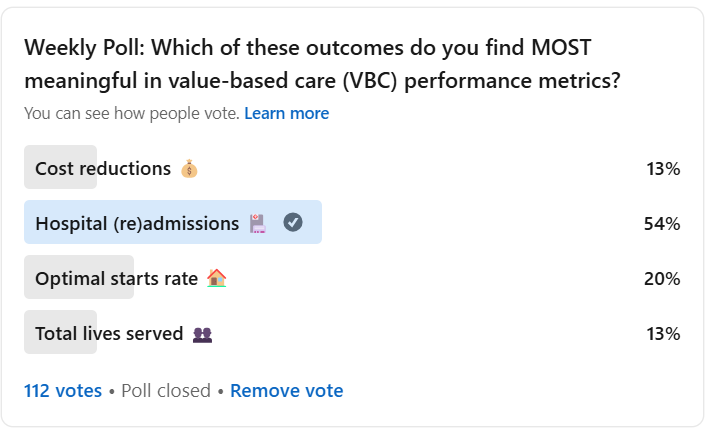
5. Which of these value-based kidney care outcomes do you find MOST meaningful?
Summary: The majority of respondents (54%) selected "Hospital (re)admissions" as the most meaningful outcome in value-based kidney care (VBC) performance metrics, highlighting the significant impact hospitalizations have on patient outcomes and healthcare costs. Other responses included "Optimal starts rate" (20%), "Cost reductions" (13%), and "Total lives served" (13%). It's worth noting that an outsized number of respondents in the latter categories may not have been directly involved in healthcare, kidney care, or VBC, which could have inflated those numbers and slightly deflated the emphasis on readmissions. [Link to poll here.]
Thoughts: Hospital readmissions are major cost drivers. That’s why so many of us focus on solutions—whether it’s delivery and payment models, devices, drugs, or digital health—that aim to prevent them. Dialysis patients, on average, spend 11 days in the hospital annually, contributing to over $14 billion in Medicare expenditures. As Anne and Qasim pointed out, hospital admissions are linked to other key metrics like cost reductions and optimal starts. Josh D. added that improving patients' starting health through better optimal starts can reduce hospital admissions, lower costs, and improve outcomes. Prioritizing optimal starts not only enhances quality of life but also minimizes hospitalizations, benefiting both patients and the healthcare system.
6. The results from the first performance year of the Kidney Care Choices (KCC) model are in. The outcomes were ___________.
Summary: A majority of respondents (58%) felt that the first-year results of the Kidney Care Choices (KCC) model were in line with expectations. Another 25% thought the outcomes were worse than expected, while 13% found them better than anticipated. The responses highlight a mixed but largely hopeful view of the model’s impact thus far. [Link to poll here.]
Thoughts: While the results were largely in line with expectations, it’s interesting to see the variations in responses, with some respondents noting that the model didn’t move the needle as much as they had hoped. As many of you pointed out in comments, the first year of this model was largely spent getting your feet under you, getting a handle on provider engagement, and preparing your stomachs for risk. This mirrors broader conversations about the ongoing challenges of implementing value-based care in the kidney space, especially when considering that quality measures mostly remained unchanged. The substantial increase in optimal ESRD starts and the higher patient activation scores are promising signs for the future, but there’s still much work to do. Given the model’s early stage, the real test will be whether these early results lead to sustained improvements in outcomes—particularly in transplantation and long-term care costs. This is a moment for further learning and collaboration as the model evolves.
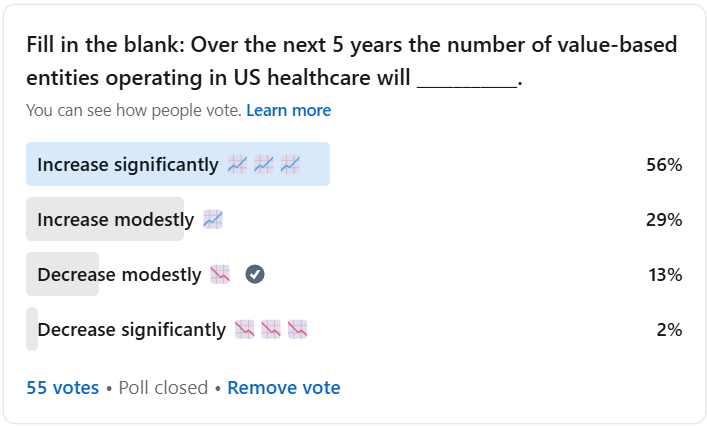
7. Over the next 5 years the number of value-based entities operating in US healthcare will (increase/decrease).
Summary: The poll results show that 56% of respondents believe the number of value-based entities in US healthcare will increase significantly over the next 5 years. A further 29% expect the increase to be more modest, while 13% anticipate a decrease, and 2% predict a significant decrease. This mirrors broader discussions about the future of value-based care and its role in reshaping healthcare systems across the country. [Link to poll here.]
Thoughts: The poll underscores the significant optimism surrounding value-based care’s future. In the context of recent reports, like the HMA study, the growth trajectory in the number of entities participating in value-based care has been remarkable, with more than a 13-fold increase since 2000. This rapid growth, combined with the maturation of the market, could lead to continued growth of value-based care organizations. However, as the market matures, we might see consolidation with leading entities acquiring others or weaker ones being phased out. As we approach 2030, it’s clear that value-based care will remain a powerful force shaping healthcare, particularly as lessons from past growth spur further innovation. The big question remains: will this momentum be enough to drive sustainable changes in care delivery and outcomes?
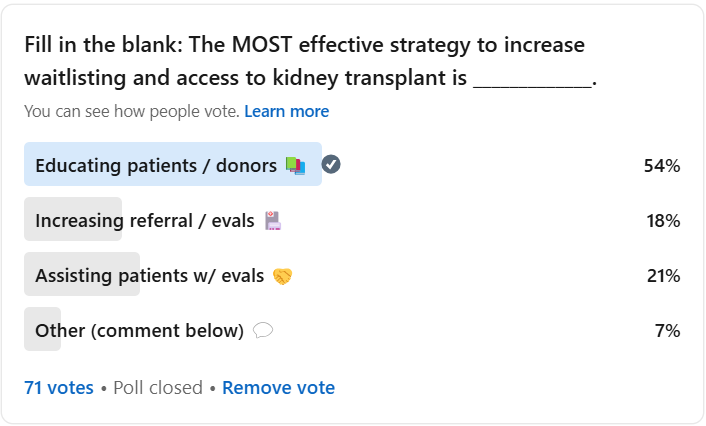
8. The MOST effective strategy to increase waitlisting and access to kidney transplant is _____________.
Summary: A majority of respondents (54%) believe that educating patients and donors is the most effective strategy to increase kidney transplant waitlisting. This was followed by assisting patients with evaluations (21%) and increasing referrals and evaluations (18%). A small portion of respondents (7%) selected "Other" with additional comments. These results highlight the critical role that education plays in bridging gaps in knowledge and increasing awareness for both potential kidney transplant recipients and donors. [Link to poll here.]
Thoughts: Educating patients and donors emerged as the clear winner, and for good reason. As highlighted in the KCC model report, communication barriers—particularly between nephrologists and transplant centers—continue to hinder progress in expanding the kidney transplant waitlist. When patients aren't properly informed or don't have the resources to navigate the process, it becomes a significant roadblock. Programs like Northwestern Memorial’s Hispanic Transplant Program demonstrate how tailored education can make a tangible difference. By engaging patients in their native language and addressing cultural misconceptions, the program not only fosters understanding but also enhances participation in the transplant process. This is a powerful reminder that breaking down barriers is often the key to unlocking better patient outcomes.
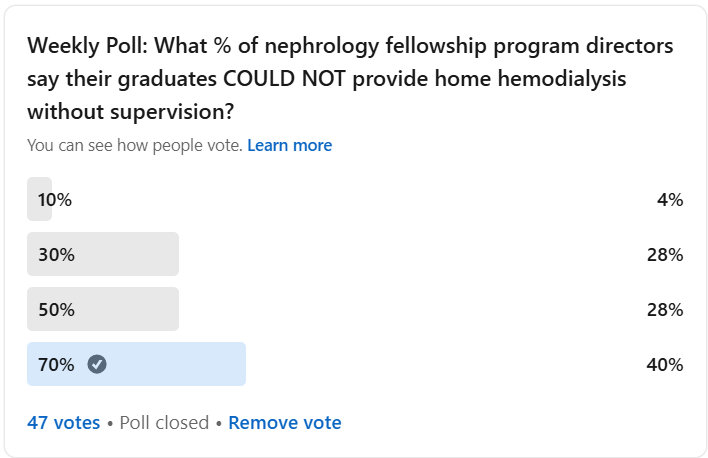
9. What % of nephrology fellowship program directors say their graduates COULD NOT provide home hemodialysis without supervision?
Summary: Only 40% of respondents correctly guessed that 70% of nephrology fellowship program directors reported that their graduates could not provide home hemodialysis without supervision. The majority of respondents (56%) selected a lower estimate, underscoring a gap in understanding the current training limitations for nephrology fellows. The survey results from Kidney Med indicate that a large portion of nephrology programs are not providing sufficient home dialysis training, signaling the need for substantial changes in fellowship curricula. [Link to poll here.]
Thoughts: This poll reflects an important gap in home dialysis training for nephrology fellows. The fact that 70% of fellowship programs graduate fellows unable to independently provide home hemodialysis highlights the need for reform in fellowship training. While initiatives like ASN’s longitudinal mentorship program and scholarships for fellows are steps in the right direction, the overall system still lacks sufficient hands-on experience in home dialysis. Addressing this gap in training is crucial for the future of kidney care, especially as home dialysis becomes more integral to treatment options.
As Qasim pointed out, we need to make prescribing home dialysis (PD/HHD) as natural as prescribing in-center dialysis, which will require both better training and greater familiarity with these treatments. Elaina also emphasized that traditional fellowships, which focus primarily on hospital-based care, often overlook home dialysis. The current system often fails to provide the time and resources needed to properly educate nephrologists on home dialysis, even though these treatments require more collaboration between the healthcare team and patients.
Adam raised an important point about the need for experienced home dialysis educators, rather than relying on physicians who may have conflicts of interest. The key to success in promoting home dialysis is empowering patients through education, especially in early stages, to ensure long-term success.
Lastly, Jameisha shared her perspective from a nursing point of view, highlighting how home hemodialysis offers flexibility but also presents challenges with prescribing PD, which can be complex and needs adjustments over time. Collaborative care between nephrologists, nurses, and patients is crucial in fine-tuning the treatment and ensuring patients’ needs are met.
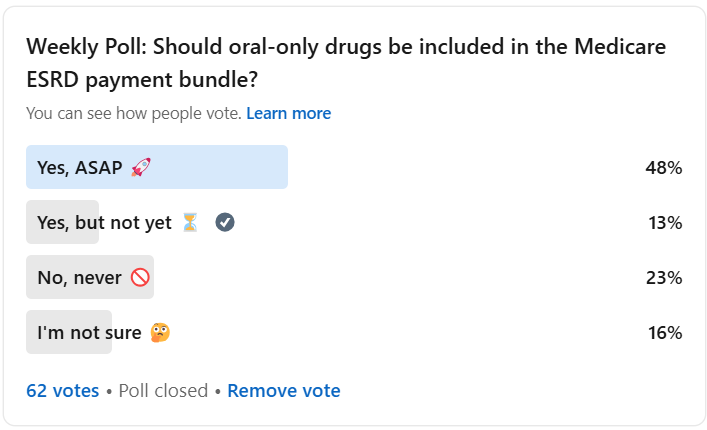
10. Should oral-only drugs be included in the Medicare ESRD payment bundle?
Summary: Nearly half (48%) of respondents believed that oral-only drugs should be included in the Medicare ESRD payment bundle "ASAP," reflecting the urgency many feel about ensuring patients have access to these critical medications. However, 23% of respondents were opposed, citing concerns about cost, while 13% prefer a delay. This aligns with recent legislative and regulatory debates over when to include oral phosphate therapies in the Medicare bundle. [Link to poll here.]
Thoughts: This question strikes at the heart of the ongoing debate over balancing cost containment with patient access to treatment. As Suresh pointed out, there are significant logistical and financial considerations from both the patient and provider perspectives. The inclusion of oral phosphate binders like Xphozah in the bundle could reduce administrative challenges in settings like nursing homes, where it's difficult to administer oral medications. However, concerns about the cost implications of bundling remain, especially if it pushes providers toward relatively low-cost alternatives.
Jeff’s comment on the trade-off between patient convenience and cost is an important one. While the lower pill burden of newer oral drugs is a significant benefit for patients, bundling may incentivize the use of cheaper alternatives that require patients to take many more pills. The question remains: can we justify sacrificing patient convenience for the sake of cost containment?
That said, it’s almost a moot point now. Last month, three months after this poll went out, CMS announced that oral-only drugs will be added to the ESRD payment bundle starting January 1, 2025.
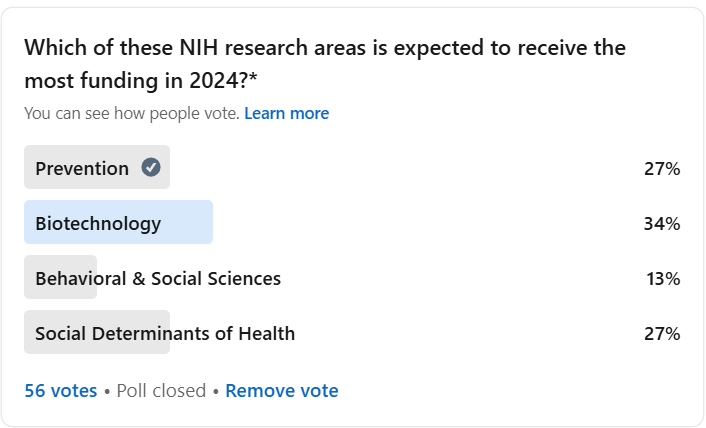
11. NIH research areas is expected to receive the most funding in 2024?
Summary: A third (34%) of respondents believe biotechnology will receive the most funding in 2024, closely followed by prevention (27%). The NIH’s FY22 funding levels support this, with biotechnology at $8.6 billion and prevention at $10.95 billion. Behavioral & Social Sciences and Social Determinants of Health (SDOH) received less attention in the poll but remain critical research areas. This funding data, from the NIH's Research, Condition, and Disease Categorization (RCDC), highlights where public investment in healthcare research is heading. [Link to poll here.]
Thoughts: The poll results highlight the growing recognition of biotechnology research, but we must also consider how funding aligns with society’s most pressing health needs. Dr. Deidra Crews, in her President’s Address at ASN Kidney Week, made a powerful point about the stark gap in public investment in kidney disease research. While the field has made significant strides, kidney health still lacks adequate funding relative to its burden on society. As Dr. Crews emphasized, advancing kidney research requires a coordinated effort to secure funding across all research phases— from basic science to implementation research— to ensure therapies reach the people who need them most.
This aligns with the concern about underfunded areas like Social Determinants of Health (SDOH), which Alice Wei pointed out. Because SDOH intersects with prevention and behavioral sciences, research in this space could influence policies with far-reaching effects on health outcomes and healthcare costs. Alice also noted that while biotechnology is crucial, it would be ideal if it were focused more on prevention. This type of research could help us better address kidney disease before it reaches its most critical stages, ultimately improving long-term health and reducing the burden on the healthcare system.
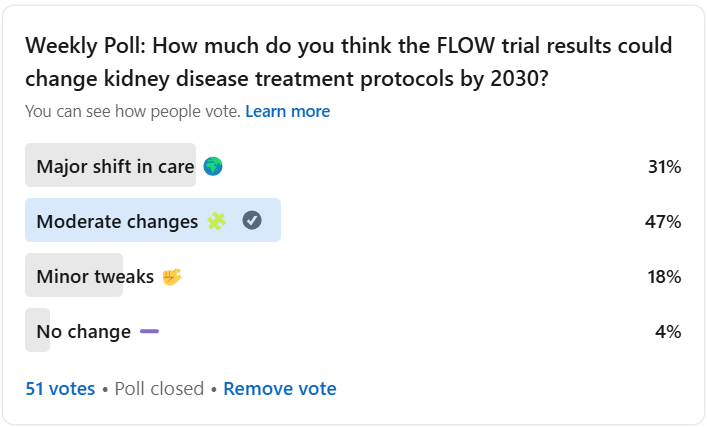
12. How much do you think the FLOW trial results could change kidney disease treatment protocols by 2030?
Summary: The majority of respondents (47%) believe the results from the FLOW trial will lead to moderate changes in kidney disease treatment protocols by 2030. Only 31% felt that the changes would be a major shift, while 18% thought they would be minor tweaks. [Link to poll here.]
Thoughts: The FLOW trial results have the potential to shift how we treat chronic kidney disease in patients with type 2 diabetes. Novo Nordisk’s findings show that semaglutide (Ozempic) significantly reduces the risk of kidney disease progression and cardiovascular events. With diabetes affecting around 30 million people in the U.S., and 40% of them suffering from kidney disease, the potential to reduce both kidney and heart disease progression could have a profound societal impact.
However, as Maria and Paul noted, concerns about cost and accessibility may limit the widespread adoption of these treatments. Without insurance coverage, these drugs can cost someone as much as $1,000 a month. These barriers could slow down the positive changes the trial suggests, but there’s hope that progress will continue. Recent data from Beth Israel Deaconess Medical Center (BIDMC) suggest that up to 137 million American adults could benefit from semaglutide, whether for weight loss, diabetes management, or preventing cardiovascular events. Despite the promise, the growing concern over the cost of GLP-1s remains. The drugs could become one of Medicare’s most expensive medications, with spending potentially increasing by up to $145 billion annually if broader eligibility definitions are applied.
As we push for greater access, the Biden-Harris Administration’s proposed rule to expand coverage of GLP-1s in Medicare and Medicaid could play a crucial role. This could reduce out-of-pocket costs for millions of beneficiaries, making these life-changing treatments more accessible. Yet, the need for equitable access is clearer than ever, as we continue to weigh the benefits against the financial and logistical hurdles that still remain. If these challenges are addressed, the landscape of kidney disease care, especially for those with type 2 diabetes, could be transformed in the next decade.
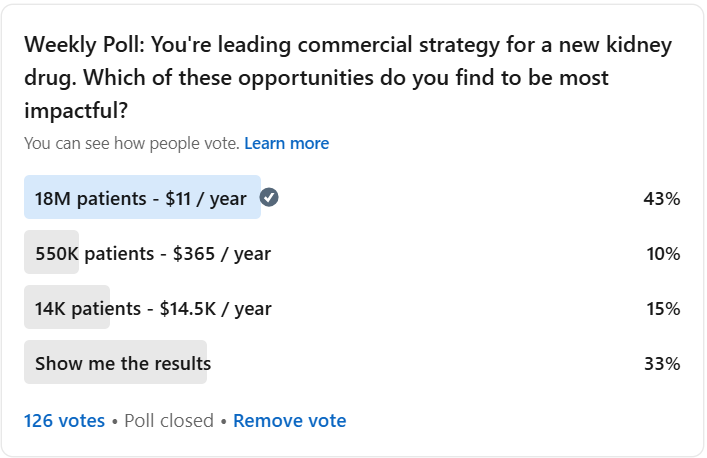
13. You're leading commercial strategy for a new kidney drug. Which of these opportunities do you find to be most impactful?
Summary: The majority of respondents (43%) believe that reaching 18 million patients at $11/year would be the most impactful commercial strategy for a new kidney drug. This aligns with the strategy employed by SGLT2 inhibitors, which target large patient populations with affordable treatments. Other respondents favored targeting smaller, high-need populations at higher price points, with 15% opting for 14K patients at $14,500/year, and 10% choosing 550K patients at $365/year. These choices reflect the balance between reach, financial return, and addressing unmet needs. All three of these idealized commercial paths net a similar annual return of around $200 million. [Link to poll here.]
Thoughts: The poll reflects the inherent tension in kidney drug commercialization: how to balance access with cost and unmet need. SGLT2 inhibitors, for instance, cast a wide net, offering treatments to millions at an affordable cost. On the other hand, GLP-1 agonists, which target smaller populations with higher price points, bring up the issues we discussed above around long-term sustainability—who ultimately pays for these expensive treatments?
Drugs targeting high-need populations, such as those for IgA nephropathy or transplant immunosuppressants, operate in a different space, commanding higher prices due to their specialized nature. All of these strategies have their merits, but each comes with its own set of challenges, including questions of equity, access, and the long-term sustainability of the pricing models. As the pipeline for kidney treatments continues to grow, these conversations are essential for understanding how market dynamics will shape the future of care. I’m currently taking this free 16-week online course from MIT on the Science and Business of Biotechnology— it’s fascinating!
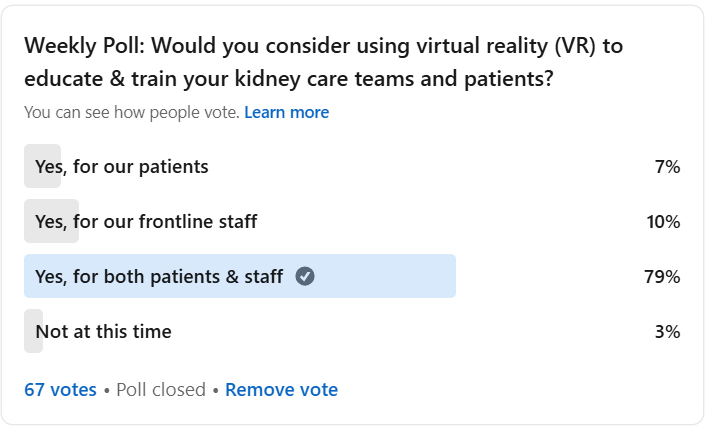
14. Would you consider using virtual reality (VR) to educate & train your kidney care teams and patients?
Summary: A strong 79% of respondents would consider using virtual reality (VR) to educate and train both kidney care teams and patients. 7% would consider it for patients only, while 10% are interested in it for frontline staff only. [Link to poll here.]
Thoughts: There’s a clear interest in utilizing VR to address key education and training challenges in kidney care, especially for patients and staff. VR has significant potential to overcome barriers such as patient fears of self-cannulation, the low uptake of home dialysis, and ongoing staffing shortages. It offers scalable, on-demand training solutions that could be a game-changer for both patients and care teams, particularly as newer devices and care models continue to emerge.
By addressing these critical gaps in education and training, VR could accelerate the adoption of home-based therapies, helping to meet national goals and alleviate the challenges faced by many dialysis centers. However, as the poll results show, the true impact will depend on how these tools are implemented and adapted to the unique needs of both providers and patients. While the future is promising, it’s essential that we continue fine-tuning these technologies to ensure they deliver real, lasting change.
Of course, none of this should surprise you if you’ve followed my work and writing over the past seven years. Colleagues and I have published our thoughts and scientific frameworks on these topics in leading journals and even built a company to bring these tools to life.
Predictions
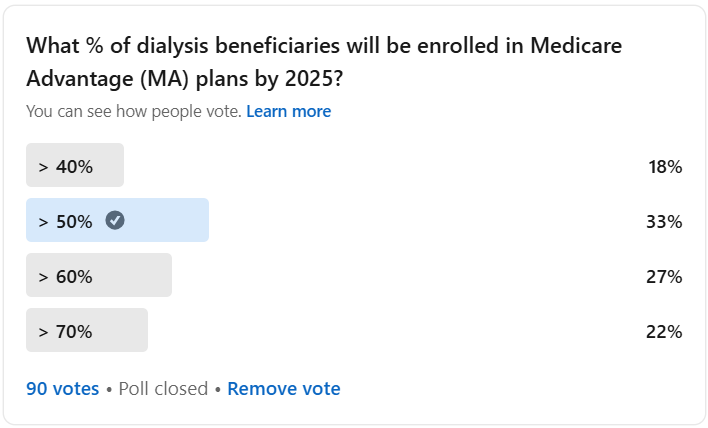
15. What percentage (%) of dialysis beneficiaries will be enrolled in Medicare Advantage plans by 2025?
Summary: The largest percentage of respondents (33%) predict that more than 50% of dialysis beneficiaries will be enrolled in Medicare Advantage (MA) plans by 2025. This prediction aligns with recent data showing rapid growth in MA enrollment among dialysis patients. As of December 2022, nearly 47% of dialysis beneficiaries were already enrolled in MA, with the number expected to continue rising. [Link to poll here.]
Thoughts: The shift to Medicare Advantage for dialysis beneficiaries is accelerating faster than expected. While MA plans offer patients more flexibility, they also face mounting financial pressures. McKinsey’s recent report indicates that payers are dealing with negative margins and may reduce benefits or increase premiums as they work to return to sustainable margins.
For kidney patients, especially those receiving dialysis, the impact could be significant. With more beneficiaries enrolling in MA plans, independent dialysis providers will need to adapt to these changes, balancing patient needs with the evolving payment structures. As the market matures, ensuring that these plans deliver quality care and that financial pressures don’t compromise patient outcomes will be critical. This shift in coverage is not just a policy change—it could fundamentally change the way kidney care is delivered and accessed.
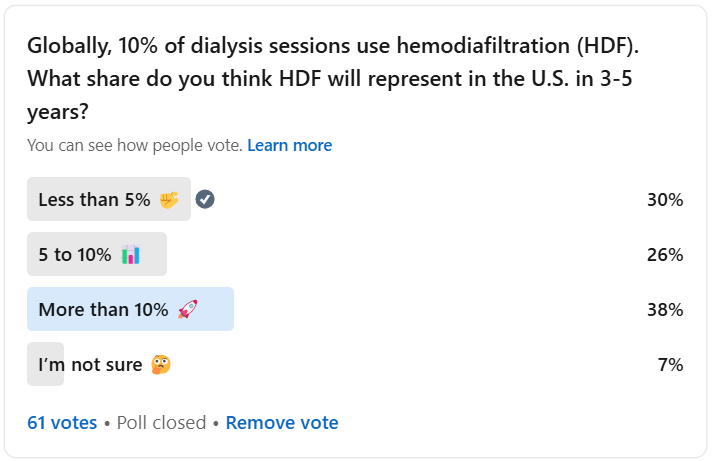
16. Globally, 10% of dialysis sessions use hemodiafiltration (HDF). What share do you think HDF will represent in the U.S. in 3-5 years?
Summary: The largest portion of respondents (38%) believes that Hemodiafiltration (HDF) will represent more than 10% of dialysis sessions in the U.S. in the next 3-5 years. HDF currently accounts for about 10% of dialysis sessions globally, but its use in the U.S. has been limited by regulatory barriers and a lack of necessary equipment. Recent studies suggest that HDF could significantly improve patient outcomes, particularly by reducing cardiovascular and all-cause mortality. [Link to poll here.]
Thoughts: Hemodiafiltration (HDF) is gaining attention as a potential game-changer in dialysis, with recent studies showing its promise in improving patient outcomes. As Dr. Katie Westin Kwon highlighted, HDF technology was a focal point at Kidney Week 2024, with significant discussions on the benefits of HDF, including a meta-analysis that showed improvements in both all-cause and cardiovascular mortality. These results, coupled with updates on cost-effectiveness and patient-reported outcomes, provide a solid case for considering HDF as a mainstream clinical option.
However, widespread adoption of HDF in the U.S. faces challenges. Regulatory barriers and a lack of appropriate dialysis machines have historically limited its use, despite HDF accounting for roughly 10% of dialysis sessions globally. In regions like Europe and the Middle East, HDF is already more common, with up to 23% of European patients receiving HDF.
Dr. Kwon also noted that while sustainability concerns, like increased water use for replacement fluids, exist, the long-term benefits of HDF—including fewer hospitalizations and reduced medication costs—could help offset the initial costs. This suggests that with the right infrastructure and investment, HDF has the potential to become a more widely adopted treatment in the U.S., especially as Fresenius considers its strategy to expand HDF worldwide.
As HDF continues to gain traction, it’s clear that its adoption could transform dialysis care, benefiting both patients and the broader healthcare system. The road to widespread implementation will require overcoming key barriers, but the evidence so far makes a compelling case for its potential.
Wrapping up
The insights from these polls highlight the complexity and opportunities in kidney care, from advancements in treatments like HDF and semaglutide to the ongoing challenges in training, accessibility, and value-based care.
As we look toward the new year, I’m excited for more polls, discussions, data, and stories that will continue to shape our understanding of kidney health. I’d love to hear from you if there are any topics or conversations that are top of mind. Your feedback and insights are always appreciated as we work together to drive progress in the field.
And, if you’re not already part of our growing Slack community, join us where we dive deeper into these questions each week with peers from industry, academia, advocacy, policy, and investment. Let’s continue to drive progress together in 2024!
Shep Glazer, a dialysis patient and vice president of the National Association of Patients on Hemodialysis (NAPH), played a pivotal role in the fight for kidney disease entitlements. In 1971, during U.S. Congressional hearings on national health insurance, Glazer made a powerful statement about the personal struggles of dialysis patients, including his own financial hardship. His most dramatic moment came when he underwent dialysis before the House Ways and Means Committee, a move that received widespread media attention and is believed to have been decisive in the passing of kidney disease entitlement legislation. This moment marked a turning point in the national conversation about dialysis and kidney care. The US Social Security Amendments of 1972 extended universal Medicare coverage to individuals with End Stage Kidney Disease who need either dialysis or transplantation to maintain life. Learn more here.
![Signals From [Space]](https://substackcdn.com/image/fetch/w_80,h_80,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F55686857-6b99-45a6-ac0f-09c9f023f2a0_500x500.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/e_trim:10:white/e_trim:10:transparent/h_72,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F4d588ac1-7fac-4bd4-829d-fc7b4e8f1326_1512x288.png)

![Signals From [Space]](https://substackcdn.com/image/fetch/w_36,h_36,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F55686857-6b99-45a6-ac0f-09c9f023f2a0_500x500.png)