Signals Recap: Humana-Monogram, FDA Approves Xeno Trials, Travere Targets FSGS, National Donor Day, & More...
Your collection of news, research, funding & community voices shaping the future of global kidney health
Welcome back. The kidneyverse has been buzzing with major developments these past two weeks, both in headlines and behind the scenes. That’s why we’re here—to bring you up to speed and open the floor for discussion.
Today, we’re diving into Humana’s expanded in-home kidney care program, the FDA’s approval of xenotransplant trials, the fourth pig kidney transplant milestone, and new insights on the rising transplant waitlist—plus marking National Donor Day and highlighting the latest in news, research, policy, and funding.
A warm welcome to the 200 new subscribers who joined us last month to help shape the future of kidney health. And a huge thank you—Signals is now a Substack bestseller! 110 posts and 18 months in, we’re building the only media-research platform dedicated to kidney innovation, and that’s because of you.
If you find this newsletter valuable, consider sharing it with 1-2 colleagues or friends who care about the future of kidney health. As always, thank you for being here, and keep exploring.
In this issue
Humana expands in-home kidney care amid MA headwinds
FDA approves first xenotransplant trials for kidney patients
New milestone: The fourth pig kidney transplant performed
Researchers create 1,000-gene map tied to kidney disease
Congress investigates one-sided kidney trade allegations
MediBeacon’s GFR monitor gets FDA approval
Trump 2.0: Health policies that could reshape kidney care
Epic and Donate Life America partner on donor registration
NephPearls: A new toolkit for RAASi therapy optimization
NKF breaks down new administration policies for kidney care
ISN partners with African nephrologists on kidney health
Travere’s next planned FDA submission targets FSGS
Visual: Kidney transplant waitlist trends over time
Open roles around the Kidneyverse
& more…
ICYMI
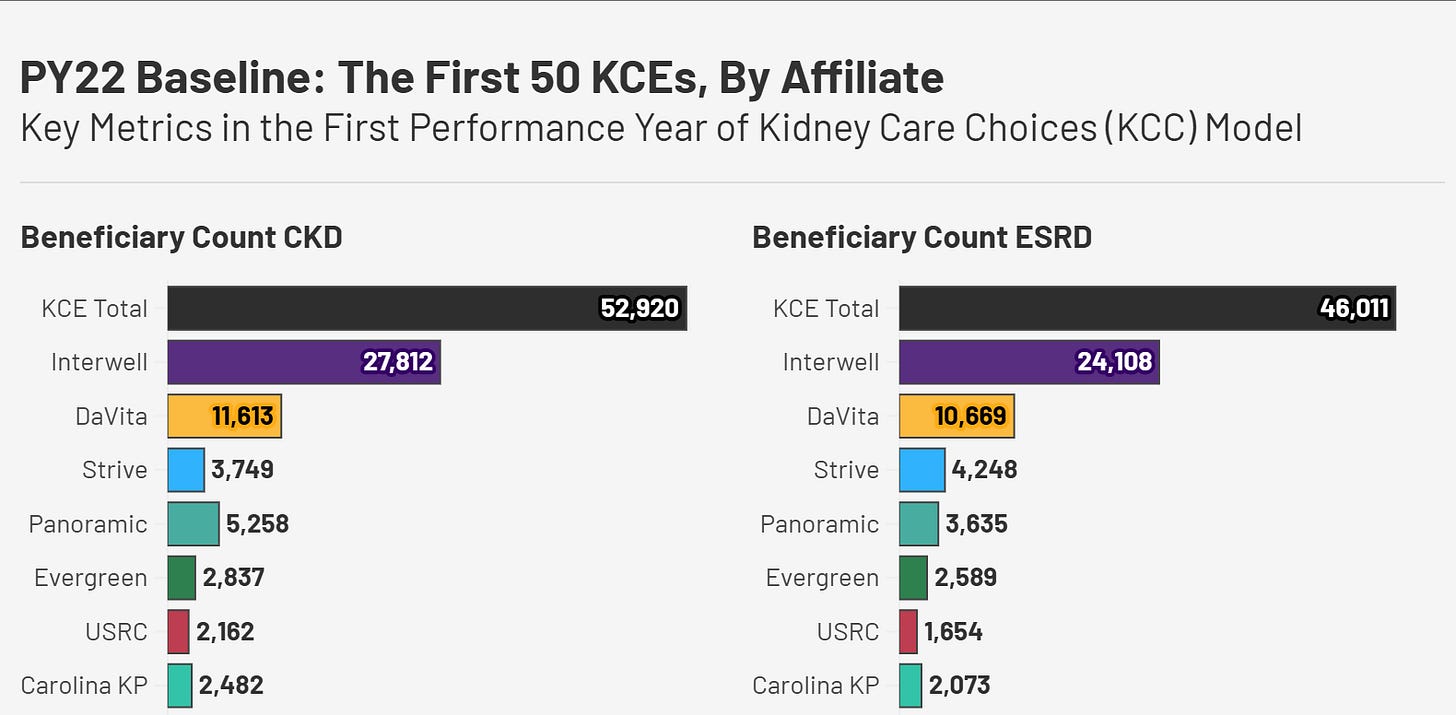
KCC in Numbers: What We Know, What We Don't, and What Comes Next. Our latest post revisits data from the first performance year (PY22) of the Kidney Care Choices model. We highlight key demographic, operational, and financial metrics across 10 affiliated care coordination organizations. We turned the post into a single-page PDF in case it’s helpful. Feel free to open and download it from the data room below.
Signals
Humana Expands In-Home Kidney Care Amid MA Headwinds
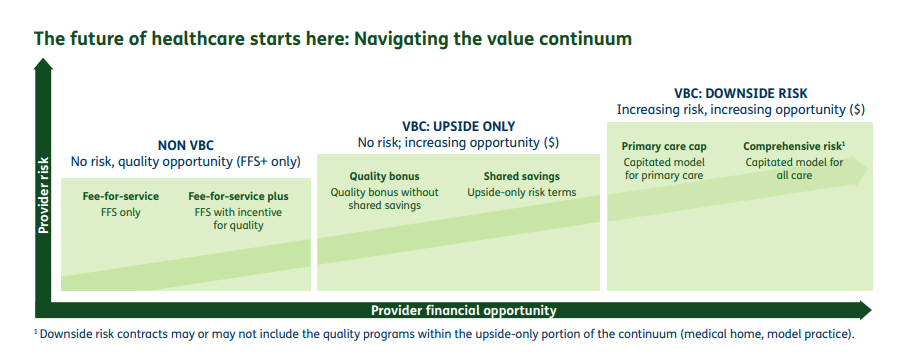
Summary: Humana and Monogram Health are expanding their in-home kidney care program to Georgia, building on their existing partnership in Alabama, Louisiana, Mississippi, and Tennessee. This move aims to provide earlier interventions for eligible Medicare Advantage members with chronic kidney disease (CKD) and end-stage kidney disease (ESKD), particularly in underserved areas. The expansion aligns with Humana’s broader push into value-based care (VBC), as detailed in its 11th annual VBC report. The report underscores the role of Medicare Advantage in accelerating VBC adoption, highlighting improved outcomes, reduced hospitalizations, and financial incentives for providers. Humana continues to advocate for expanding VBC into Medicaid, emphasizing its potential to enhance chronic disease management and health equity. We covered Humana’s value-based kidney care report last year, which at the time had impacted over 77,000 patients nationwide, with notable improvements in unnecessary hospital admissions, MER, and rates of nephrology follow-up visits.1
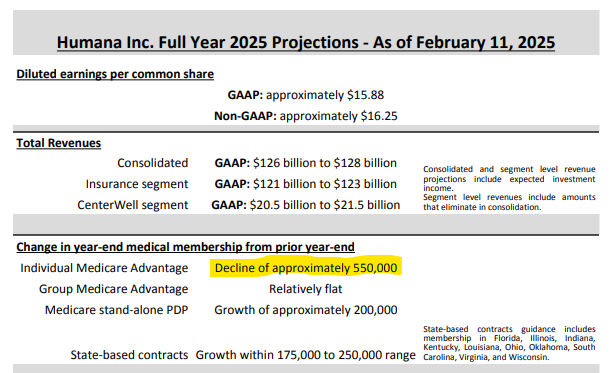
Thoughts: Humana’s expansion with Monogram comes as the insurer navigates financial and operational headwinds, including a projected 10% decline in Medicare Advantage (MA) membership in 2025 (~550,000 members) and the impact of lower Star Ratings on future bonus payments. Despite these challenges, Humana continues to bet on value-based care (VBC) and in-home polychronic care as part of its long-term strategy. Its latest earnings call highlighted a focus on managing medical spending, improving patient and provider engagement, and driving profitable growth—all areas where home-based kidney care could play a role. Meanwhile, CMS’s first-year Kidney Care Choices (KCC) evaluation showed mixed-positive results, reinforcing the complexities of managing CKD and ESRD populations under risk-based models. As Humana and others double down on MA-driven VBC, the key question remains: Can these models scale effectively and deliver sustained improvements in cost and care outcomes?2
What do you think? What do people not know or misunderstand about Medicare Advantage, public or private ESRD costs that they should?3
FDA Approves First Xenotransplant Trials for Kidney Patients

Summary: The FDA has approved clinical trials for two biotech companies, United Therapeutics and eGenesis, to transplant genetically modified pig kidneys into patients with kidney failure. United Therapeutics will begin with six patients, potentially expanding to 50, while eGenesis will start with three patients who are unlikely to receive a human kidney within five years. These trials mark a major step toward xenotransplantation, which could help address the severe organ shortage—nearly 100,000 Americans are currently on the kidney transplant waitlist. However, questions remain about long-term safety, immune response, biosecurity, and ethical concerns. Meanwhile, the fourth xenotransplant just took place, with Tim Andrews, a 66-year-old dialysis patient, receiving a pig kidney at Massachusetts General Hospital. His transplant team shared that Andrews had just a 9% chance of receiving a human kidney in the next five years and a nearly 50% chance of being removed from the waitlist due to declining health.
Thoughts: Xenotransplantation is moving from experimental surgeries to structured clinical trials, and the implications are massive. If these trials prove successful, we could be on the verge of a major shift in organ availability. But will it be enough? Many in the kidney community remain skeptical that “xeno” alone will meaningfully reduce the transplant waitlist in the near future. In my recent poll, nearly half of respondents predicted the waitlist would be longer in 10 years than it is today. Even with advancements in xenotransplantation, bioengineering, and donor incentives, rising rates of diabetes, hypertension, and kidney disease could outpace these innovations. The reality is that no single breakthrough will solve the organ shortage—it will take a combination of new therapies, better prevention, and systemic policy changes.
What is you biggest hope for transplant by the end of 2025?
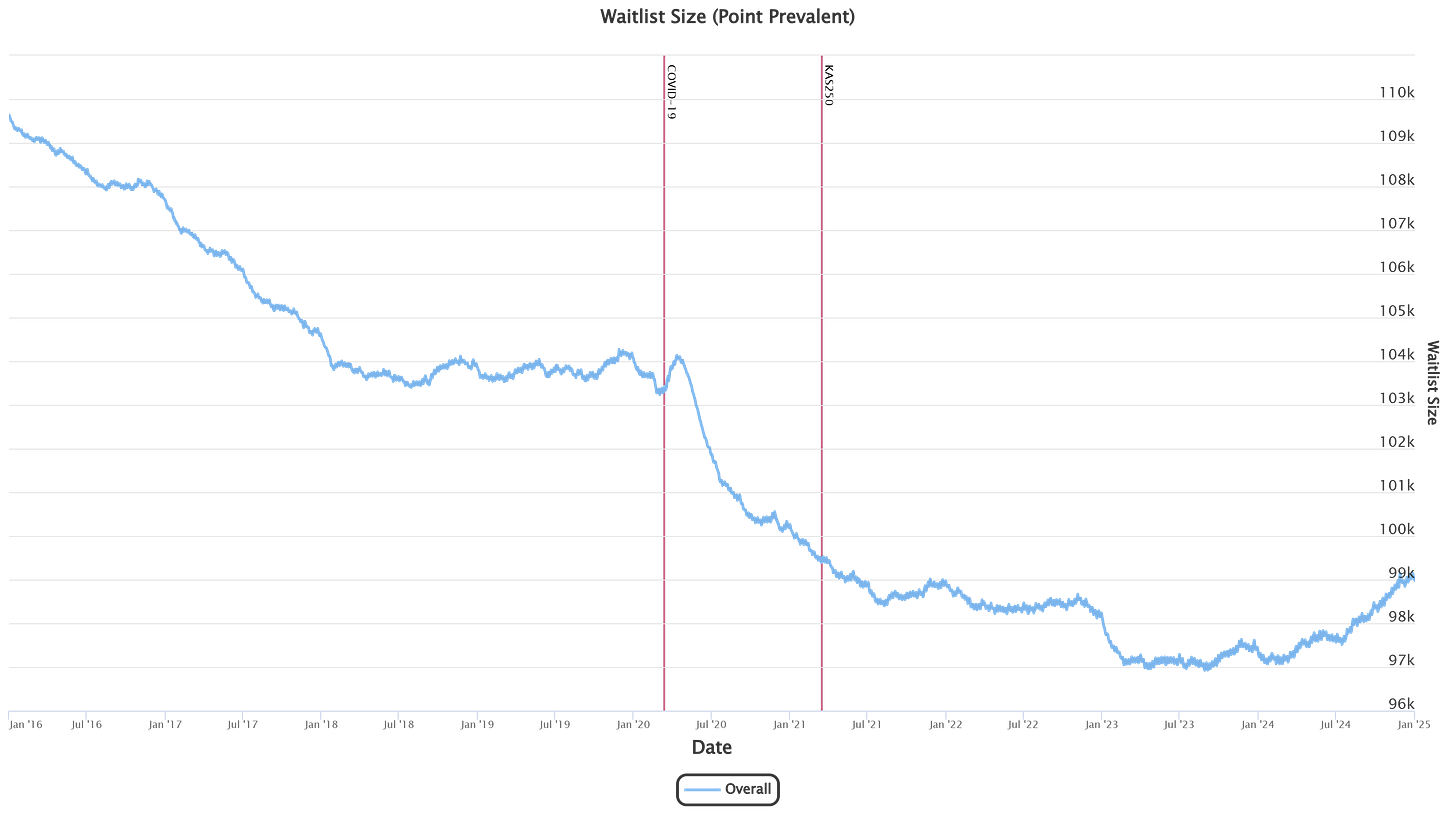
Visual of the Week
Kidney Transplant Waitlist Size, 2016 to Present. After years of decline, the kidney transplant waitlist has started growing again. This chart tracks the total number of people on the waitlist on each day over time, with key policy changes and the onset of COVID-19 marked by vertical lines. The newest kidney allocation policy (“KAS250”) broadened geographic distribution while increasing allocation system complexity.4 The long-term downward trend reversed in 2022, and the waitlist has been steadily climbing ever since.
Recent discussions in the kidney community reflect uncertainty about where this trend is headed. In my latest poll, nearly half of respondents predicted the waitlist will be longer in 10 years than it is today. While some see hope in xenotransplantation, organ bioengineering, and living donor incentives, others believe rising rates of kidney disease and systemic barriers to transplantation will outweigh these innovations.
What do you think—will the waitlist be longer or shorter in 2035? What factors will make the biggest impact?
News

eGenesis Announces A Fourth Person Has Received a Pig Kidney Transplant [TIME]
Humana and Monogram Health Announce Expansion of Comprehensive Kidney Care Program in Alabama, Louisiana, Mississippi, Tennessee, and now Georgia [Press Release]
Travere Therapeutics to Submit sNDA for FILSPARI® (sparsentan) in FSGS [Press Release]
Congresswoman Jill Tokuda demands answers after news investigation exposes one-sided kidney trade [Hawaii News Now]
Researchers create the most complete genetic map tied to kidney disease, with more than 1,000 genes that influence kidney function [Penn Today]
Epic and Donate Life America (DLA) are collaborating to offer patients a seamless way to register as organ, eye and tissue donors directly through MyChart. [Press Release]
MediBeacon Transdermal GFR System Receives FDA Approval to Assess Kidney Function [Press Release]
Junevity Raises $10M to Develop Cell Reset Therapeutics for Longevity, with an Initial Focus on Type 2 Diabetes, Obesity and Frailty [Press Release]
Heather Knight has been appointed to the newly created role of Chief Operating Officer at Baxter International. [LinkedIn]
Trump 2.0: Scott Alexander wrote an interesting piece about what new health policies might look like in a ~90th percentile best outcome scenario. He covers paying organ donors, better longevity biomarkers, Warp Speed for air quality, and improved FDA transparency to name a few. [Astral Codex Ten]
Discussion about NIH research funding cuts requires 'data, time and careful evaluation' [Healio]
Research
OPTN/SRTR 2023 Annual Data Report: Kidney [Amer J of Transpl] (H/t Krista Lentine for sharing and leading this effort)
Researchers create genetic map tied to kidney disease
Effects of Clazakizumab on Anemia and Iron Metabolism in Patients with Kidney Failure [JASN] (H/t Brendon Neuen for sharing, and great work!)
Risk-directed management of chronic kidney disease [Nature Rev Neph]
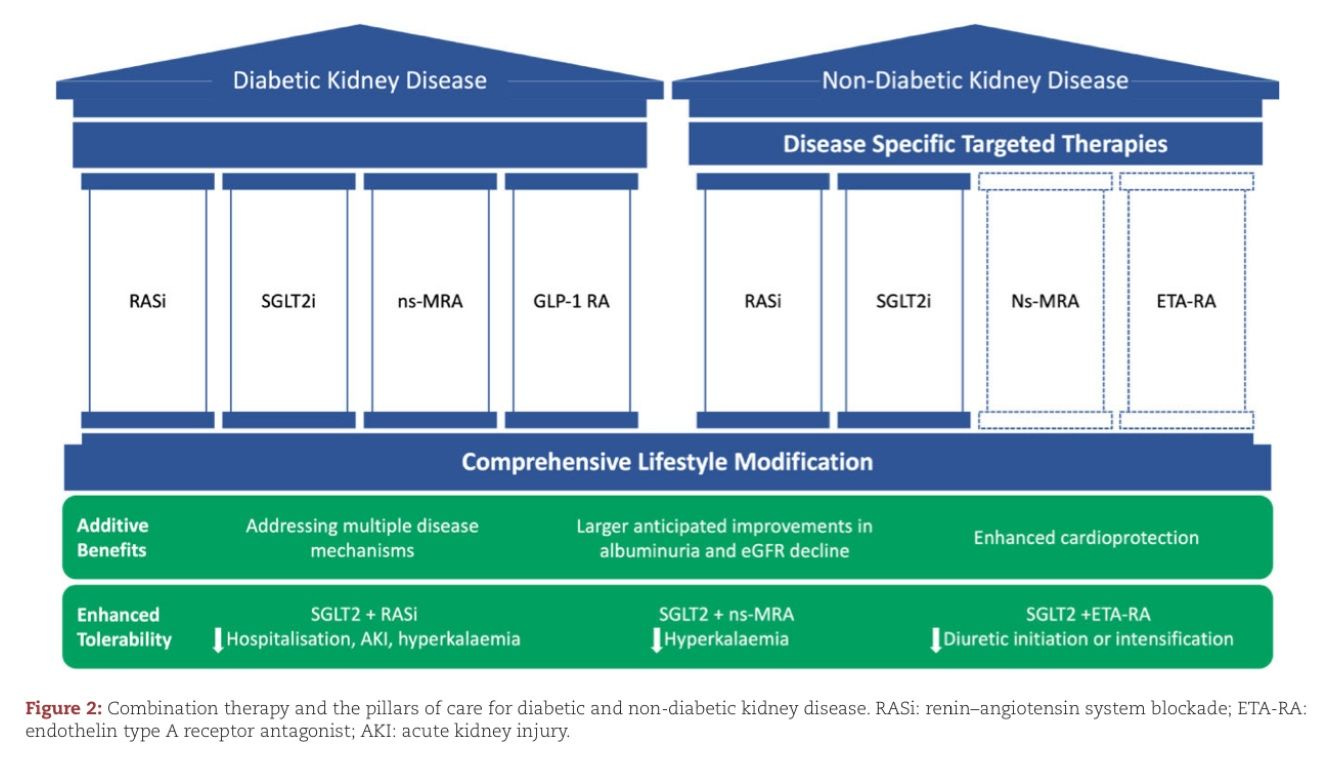
Combination therapy as a new standard of care in diabetic and non-diabetic chronic kidney disease [Nephrol Dial Transplant]
Treatment of patients with IgA nephropathy: a call for a new paradigm [Kidney Int] (H/t Davide Garrisi for sharing)
Remote management of anaemia in patients with end-stage kidney disease using a wearable, non-invasive sensor [Clin Kidney J]
The rise of agentic AI teammates in medicine [The Lancet]
NephPearls: Optimization of RAASi Therapy Toolkit [ISN] (H/t Edgar Lerma)
Community
National Donor Day: Taking a moment to recognize the incredible impact of organ and tissue donation, celebrate donors and their families, and encourage more conversations around transplant awareness. [UPMC] [Miriam] [USA Today]
Patient Voice: Dr. Patrick Gee, Sr. recently shared his perspective on the question: “Would You Consider Accepting a Pig Kidney Transplant?” [Kidney 360]
Policy: New Administration, New Policies: What It Means for Kidney Patients [NKF]
Equity: Black kidney patients find renewed hope after rules change for transplant list [ABC News]
ISN25: ISN and the African Association of Nephrology signed an MOU to partner on kidney health initiatives across the African continent. [LinkedIn] (H/t for sharing Tushar Vachharajani)
Events: 2025 Florida Kidney Day in Tallahassee on March 9-10, hosted by the Florida Renal Association [Get Tickets] (H/t for sharing Julie Spears)
ISN25: The teams at Nova Biomed and hellokidney teamed up to run a CKD screening program for attendees using the NovaMaxPro and digital health platform. [LinkedIn] (H/t Bogdan Milojkovic for sharing)
ISN25: Rolando Claure Del Granado recently shared a great post celebrating 40 years of the ISN Fellowship Program, and thanking Ravindra Mehta for his guidance.
Global: Reducing the burden of noncommunicable diseases through promotion of kidney health and strengthening prevention and control of kidney disease [World Health Organization]
Jobs
Palliative APP (Birmingham, AL) at Monogram Health
Head of Brand, Marketing, & Comms at Monogram Health
Sr. Director, Compliance & Privacy at Monogram Health
SVP Value-Based Care at Guaranteed
Hospital & Patient Services Mgr (Charlotte, NC) at Fresenius
Thought Leader Liaison, Nephrology at Mallinckrodt
Health and Home Strategy Lead at Google
Organ Health Specialist (Boston, MA) at Natera
Health Product Manager at Best Buy Health
Senior Growth PM, US Digital Health at Samsung Health
Supported By
Signals is made possible with the generous support of our sponsors. We are grateful to partner with organizations committed to advancing global kidney care innovation. This post was made possible by Roivios, the team developing the world’s first renal assist device. Thanks team!
In 2019, Humana CKD patients had a Medical Expense Ratio (MER) over 100%, but as VBC engagement has increased, MER dropped to 88% over 5 years. Learn more here.
Humana Reports Fourth Quarter 2024 Financial Results; Provides Full Year 2025 Financial Guidance (2/11/25) — press.humana.com
Humana Reports Fourth Quarter 2024 Financial Results; Provides Full Year 2025 Financial Guidance — humana.gcs-web.com
![Signals From [Space]](https://substackcdn.com/image/fetch/w_80,h_80,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F55686857-6b99-45a6-ac0f-09c9f023f2a0_500x500.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/e_trim:10:white/e_trim:10:transparent/h_72,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F4d588ac1-7fac-4bd4-829d-fc7b4e8f1326_1512x288.png)

![Signals From [Space]](https://substackcdn.com/image/fetch/w_36,h_36,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F55686857-6b99-45a6-ac0f-09c9f023f2a0_500x500.png)





There is a lot of discussion in the Dialysis space regarding Medicare advantage. Medicare advantage impacts independent Dialysis providers the most. Medicare advantage is heavily marketed to patients and patients are able to enroll on a quarterly basis. Some of the potential benefits marketed to patients is often misleading. For example, Medicare advantage plans will promise covered services, such as transportation, but transportation to dialysis is not included.
Patients are told that joining a Medicare advantage plan will not require a change of dialysis provider, but the plan rarely shows the inpatient Dialysis and Nephrology providers when marketing and selling Medicare advantage plans. Medicare advantage is also not transparent regarding patients on dialysis maximum out-of-pocket cost that they are responsible for covering.
When a traditional Medicare patient changes to a Medicare advantage plan they’re permitted to keep their Medigap secondary insurance coverage. However the Dialysis space has seen that most Medicare advantage plans advise against keeping the patients Medigap insurance. Some of the information presented to the patient advises against keeping the Medigap insurance telling patients they’re better off, directing those dollars through their out-of-pocket expenses
If the patient chooses to return to traditional Medicare, the patient must undergo underwriting, which is different in each state, to reinstate or acquire their Medigap policy. There are other multiple aspects of Medicare advantage that do not benefit the dialysis patient and provider, but too much to put here.