Signals Recap: Mass Layoffs at HHS & VA; NYT Investigates Transplant Chaos; FDA Fast-Tracks Kidney Cancer Drug & More…
Your biweekly collection of news, research, funding & community voices shaping the future of global kidney health
Welcome back! We’re kicking off Kidney Month here in the United States, and what better way to raise awareness than by bringing you up to speed on the latest news, research, policy, and discussions shaping kidney health today.
This week, we lead off with the bombshell New York Times investigation that exposes an organ allocation system ‘in chaos’ as waiting lists are ignored. We’ll break down the findings, OPO responses, and what this means for patients and transplant policy. Meanwhile, mass layoffs at HHS, the VA, and key health agencies are raising alarms across the healthcare system. Thousands of federal workers—including those at the FDA, CMS, and NIH—have been fired, sparking legal battles and concerns over long-term oversight in areas like transplantation.
Extending a warm welcome to the 221 new subscribers who joined us last month to help shape the future of kidney health. We’ve been busy these last couple of weeks. In case you missed it, we published our value-based kidney care directory, KCC PY22 results overview, and DaVita Q4 earnings snapshot. Stay tuned for our Fresenius Q4 snapshot, updated device landscape, and more KOL interviews coming soon.
If you find this newsletter valuable, consider sharing it with 1-2 colleagues or friends who care about the future of kidney health. Thank you for being here with us.
In this issue
NYT: Organ transplant system ‘in chaos’—waiting lists ignored
Mass layoffs at federal health agencies continue
Third recipient of a pig kidney heads home
Baxter Kidney Care rebrands as Vantive
FDA grants priority review to new kidney cancer imaging drug
Memorial Hermann hit with severe transplant sanctions
NephCure’s journey from small idea to major movement
JAMA paper challenges value-based payments in Medicare
Indigenous Kidney Taskforce gathers to shape future care
Congress investigates global kidney trade concerns
AI predicts kidney injury risk in emergency patients
OrganOx secures $142 million to grow metra platform
The rising cost of liver transplantation in the U.S.
New outpatient dialysis guidance for AKI patients
A new approach to vascular access saves an ESRD patient
Open roles around the Kidneyverse
& More…
This issue is made possible by Guaranteed, the company optimizing end-of-life care experiences for CKD and ESRD patients at risk-bearing nephrology practices when conservative kidney management, dialysis and kidney transplants are no longer viable options. Email raihan@onguaranteed.com today to learn more. Thank you team!
Signals
NYT: Organ Transplant System ‘in Chaos’ as Waiting Lists Are Ignored
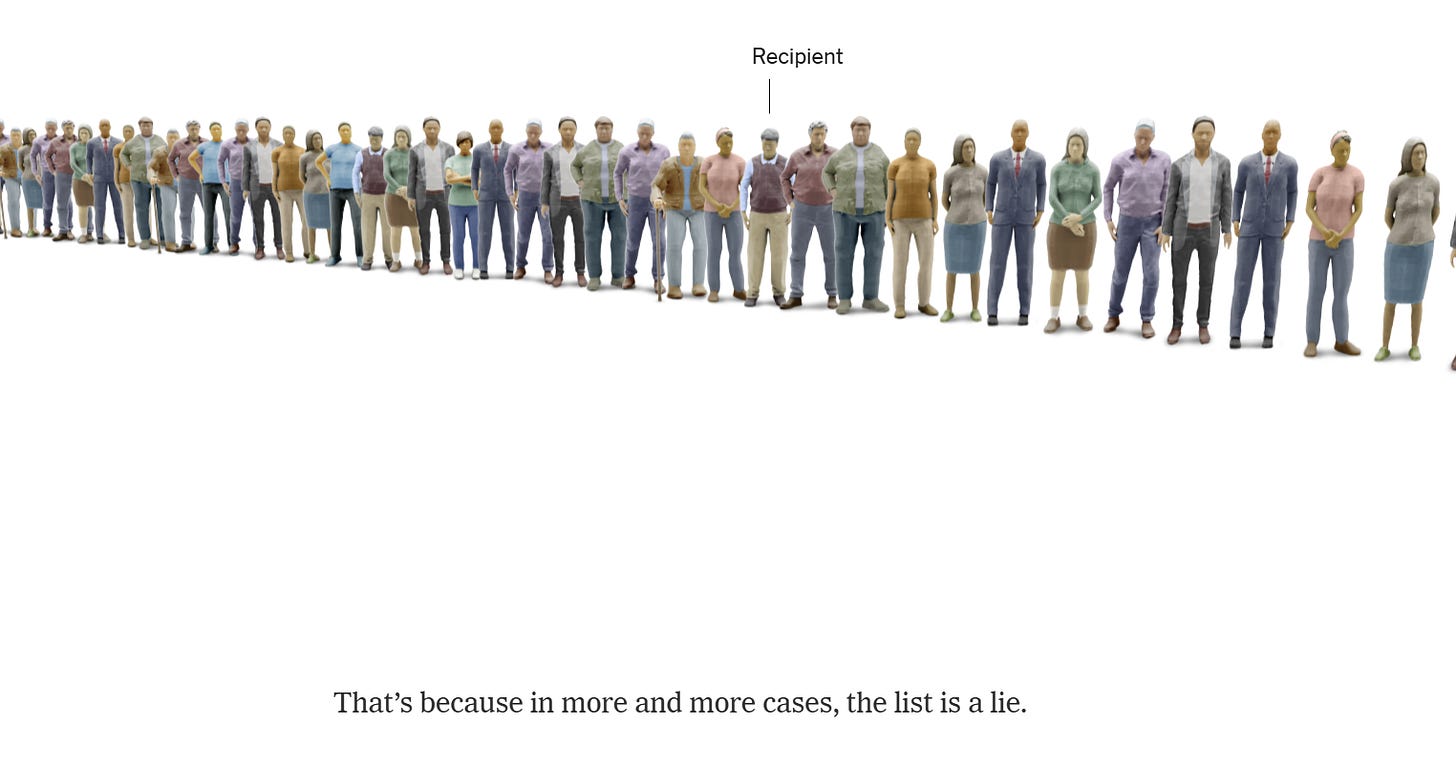
Summary: A New York Times investigation uncovered that nearly 1 in 5 organs from deceased donors in 2024 were allocated outside the standard waiting list process—a sixfold increase from previous years. The report highlights how hospitals and organ procurement organizations (OPOs) are bypassing the sickest and longest-waiting patients, often prioritizing recipients who are healthier, easier to transplant, or affiliated with certain transplant centers. While some argue these workarounds help reduce organ waste, the investigation raises serious concerns about equity, transparency, and accountability in the U.S. transplant system. Over the past five years, more than 1,200 patients died after being skipped despite being near the top of the list. The practice appears to disproportionately benefit white and Asian patients, men, and college graduates, exacerbating existing disparities in organ access. Since publication, several OPOs, including LifeGift’s CEO, have responded to the findings.
Thoughts: The transplant system relies on trust and transparency—without it, public confidence in organ donation will erode. While OPOs argue that out-of-sequence allocations prevent organ discards, the authors point out these shortcuts haven’t meaningfully reduced waste. The report highlights a lack of oversight, as regulators have largely failed to intervene despite clear deviations from policy. As Miriam puts it, the point of policy is to have policy and to almost always adhere to it. If the system now requires hospitals and OPOs to make real-time allocation decisions, it raises serious questions about governance and accountability. At the same time, as Jeanmarie noted, thousands of kidneys are still being discarded due to logistical issues despite commercially available solutions like perfusion, leaving patients in long-wait regions feeling hopeless. With xenotransplantation trials now underway, recent policy efforts like the End Kidney Deaths Act being debated, and mass layoffs in Washington, we are at a pivotal moment for the future of organ transplantation.
What do you think? Where do conversations go from here on topics like reform, transparency, and trust? What explains these outcomes?
Mass Layoffs at HHS & VA Signal a Reshaped Federal Health Landscape

Summary: A wave of mass layoffs across HHS, the VA, and key health agencies is rapidly reshaping the federal workforce, with thousands of employees terminated under the new administration’s directive to "streamline government" and eliminate "corrupt bureaucracy." While framed as a cost-cutting measure—projected to save $781 million annually—the move has sparked legal battles, labor protests, and deep concerns about its long-term impact on public health infrastructure.
A federal judge ruled some of the firings illegal, citing overreach by the Office of Personnel Management (OPM), yet stopped short of reversing them. Meanwhile, agencies have been ordered to submit reorganization plans by April, including recommendations for further mass layoffs, real estate downsizing, and relocation of headquarters to "less-costly" areas. The administration's hiring freeze remains in effect, restricting agencies to hiring only one employee for every four fired.
Fallout: Veterans' disability claims backlog worsens as VA case analysts were cut; HHS scrambled to reverse firings of FDA and Indian Health Service employees; medical AI oversight at the FDA temporarily collapsed after half the device AI team was dismissed; public health experts, epidemiologists, and CMS officials were let go, raising concerns about government preparedness; DEI and health equity programs were slashed, with entire offices put on leave and references to health disparities quietly removed.1
Thoughts: These cuts go beyond bureaucracy—they threaten the backbone of federal healthcare oversight. While the administration frames this as efficiency, gutting agencies like the FDA, CMS, and VA weakens essential services, from veterans’ care to medical innovation and public health preparedness. With more layoffs expected and litigation mounting, the long-term stability of federal health policy is at stake. The Organ Procurement and Transplantation Network (OPTN) is among the entities navigating these changes, with its interim executive director addressing concerns about how the transition is impacting operations.
I welcome your feedback and would love to hear from those of you impacted by these latest changes. In fact, I'd like to open the mic for an 'exit interview' style Q&A with anyone willing to share their experiences. Your work, expertise, and thoughts on the road ahead deserve to be heard.2
What impacts have you seen or experienced from these changes—on your work, your community, or your outlook?
Visual of the Week
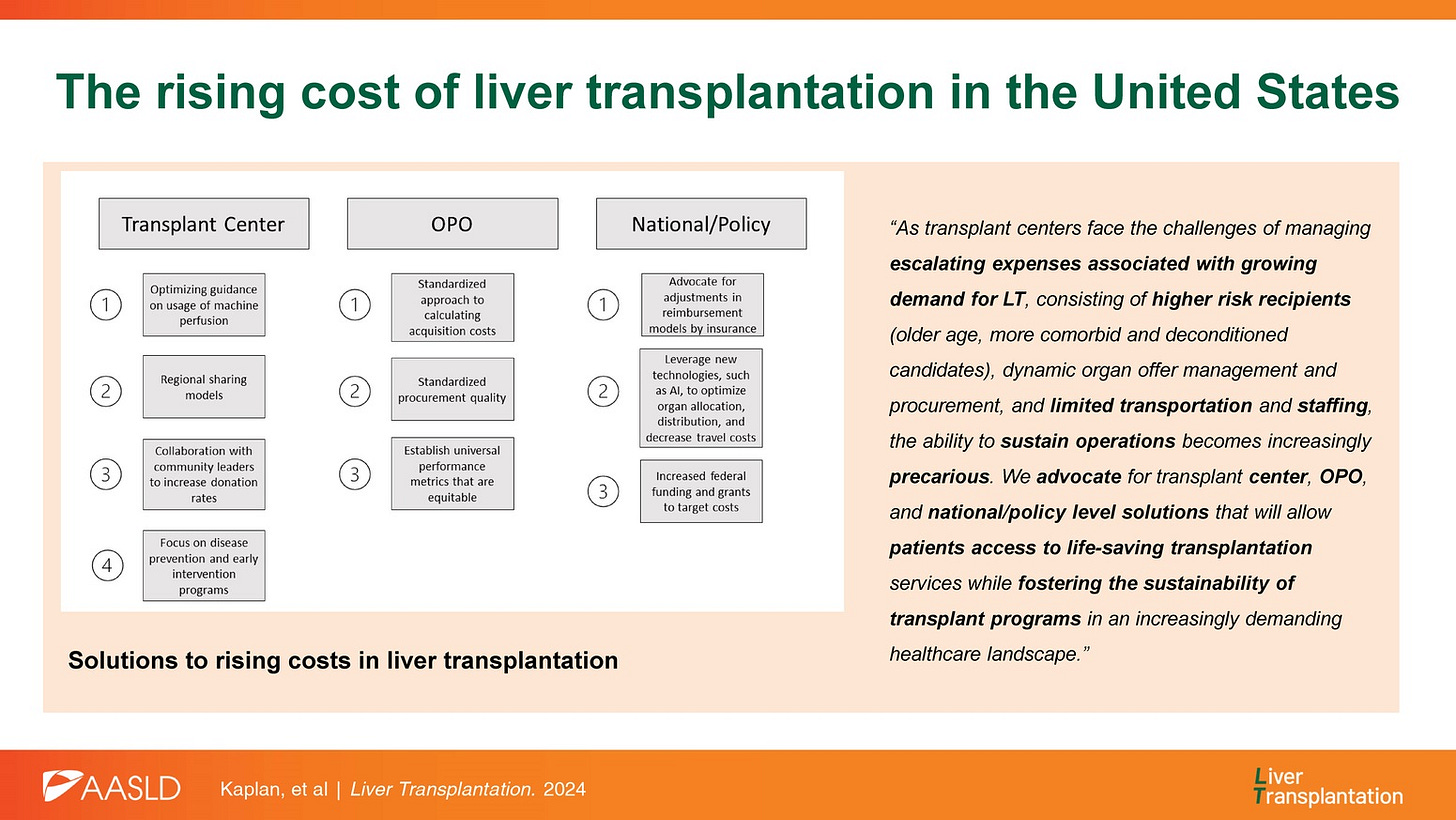
Solutions to rising costs in liver transplantation. An impressive group of co-authors from top liver transplant programs have published a review paper on the rising costs of liver transplantation. They explore how expanded criteria, broader organ distribution, and costly new technologies are straining transplant programs. Despite these rising costs, reimbursement remains stagnant, threatening program sustainability and patient access. The paper examines policy changes, OPO practices, and emerging solutions to improve efficiency, resource allocation, and financial sustainability in LT.
What do you think—which of these proposed solutions do you see as most feasible in the coming years? Which have you seen firsthand?
News

Third recipient of a pig kidney heads home from the hospital (STAT) – The latest milestone in xenotransplantation, as a patient successfully recovers post-surgery.
Baxter Kidney Care rebrands as Vantive, a new standalone vital organ therapy company (Press release).
OrganOx secures $142M equity financing for organ preservation technology platform metra (Mobihealthnews)
Fresenius sells select lab assets to Quest Diagnostics (Press release, h/t Bryan Thompson).
Paragonix successfully tests KidneyVault Renal Perfusion System in four transplants (DocWire).
FDA grants priority review to TLX250-CDx (Zircaix®) for kidney cancer imaging (Press release).
Northernmost partners with Mayo Clinic to develop NoMo Kidney Pump (Press release, h/t Ron Mills).
Memorial Hermann hit with rare, severe sanction over organ transplant scandal—investigation cites a 'culture of intimidation' (Houston Chronicle, h/t Rebecca Baranoff).
FDA removes semaglutide from its drug shortage list, confirmed in a press release by Novo Nordisk (Healio, Press release).
YMCA of the USA expands partnership with DaVita to advance kidney health in seven communities (Morningstar, h/t Paul Gordon).
Geographic gaps in kidney allocation policy leave Hawaii, Puerto Rico, and Alaska at a disadvantage (Hawaii News Now).
'Desperate' illegal kidney sales uncovered in Myanmar villages (BBC News).
Queens teacher donates kidney to a colleague—despite barely knowing each other (NBC New York).
Westmoreland County Navy veteran in search of kidney donor (ABC News)
Research
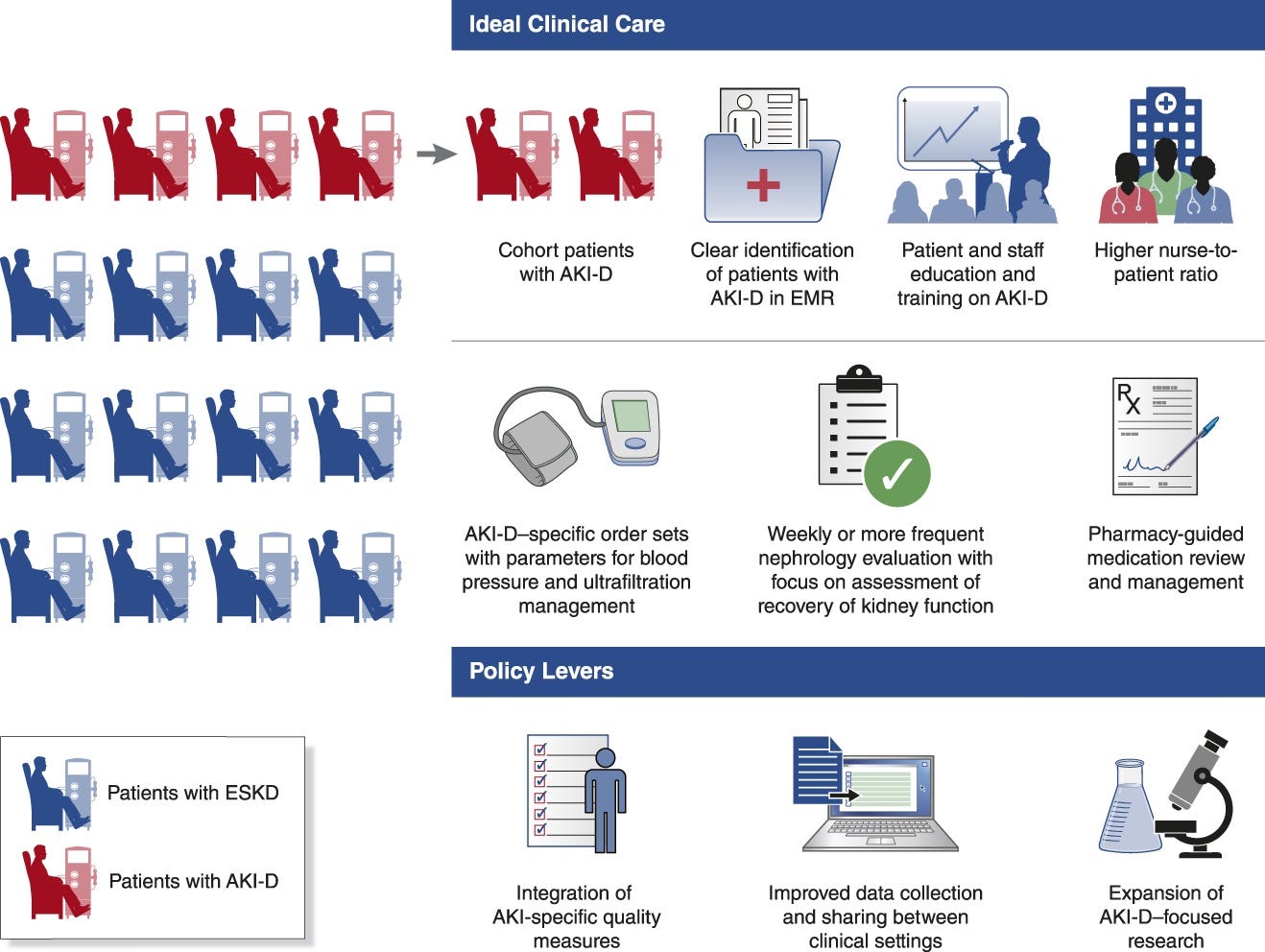
ASN Kidney Health Guidance on the Outpatient Management of Patients with Dialysis-Requiring Acute Kidney Injury (JASN, h/t Anitha Vijayan)
Prediction of contrast-associated acute kidney injury with machine-learning in patients undergoing contrast-enhanced computed tomography in emergency department (Nature)
Sleep Patterns, Symptoms, and Mortality in Hemodialysis: A Prospective Cohort Study (Kidney Medicine)
Factors affecting access to dialysis for patients with end-stage kidney disease in Sub-Saharan Africa: A scoping review (NursingOpen, h/t Bogdan M.)
Haemodiafiltration versus high-flux haemodialysis - a Consensus Statement from the EuDial Working Group of the ERA (NDT)
The rising cost of liver transplantation in the United States (Liver Transplantation, h/t Sharon Klarman)
Venous thromboembolism prevention for nephrotic syndrome: The role of aspirin, vitamin K antagonists and direct oral anticoagulants (Kidney Intl, h/t Sayna Norouzi)
Community
NYU Langone on OPTN modernization – In a new YouTube talk, Dr. Macey Levan breaks down the 2025 governance restructure of the Organ Procurement and Transplantation Network (OPTN), including the new independent board and what these changes mean for patients, providers, and the future of transplantation. (NYU Langone Health, h/t Charles Bearden)
JAMA challenges value-based payment in Medicare – A new JAMA perspective argues that value-based payment (VBP) is failing to reduce costs and is instead creating more corporate intermediaries while impeding critical Medicare reforms. The authors propose a new Medicare agenda focused on fixing, not abandoning, fee-for-service (FFS) by addressing the true drivers of high costs: technology pricing and administrative waste. (JAMA, h/t Hayden Rooke-Ley)
ABUNDANT sets world premiere in Hollywood on March 1 – The film, which explores living kidney donation, debuted yesterday. (Press Release, Website)
NephCure: From a small idea to a movement – What started with four determined families has grown into a national force driving hope, collaboration, and change for rare kidney disease patients. (LinkedIn)
Patrick O. Gee, Sr. on the power of community partnerships in research – He shared key takeaways on how leaders can collaborate with The PATIENTS Program to co-develop health initiatives. (LinkedIn)
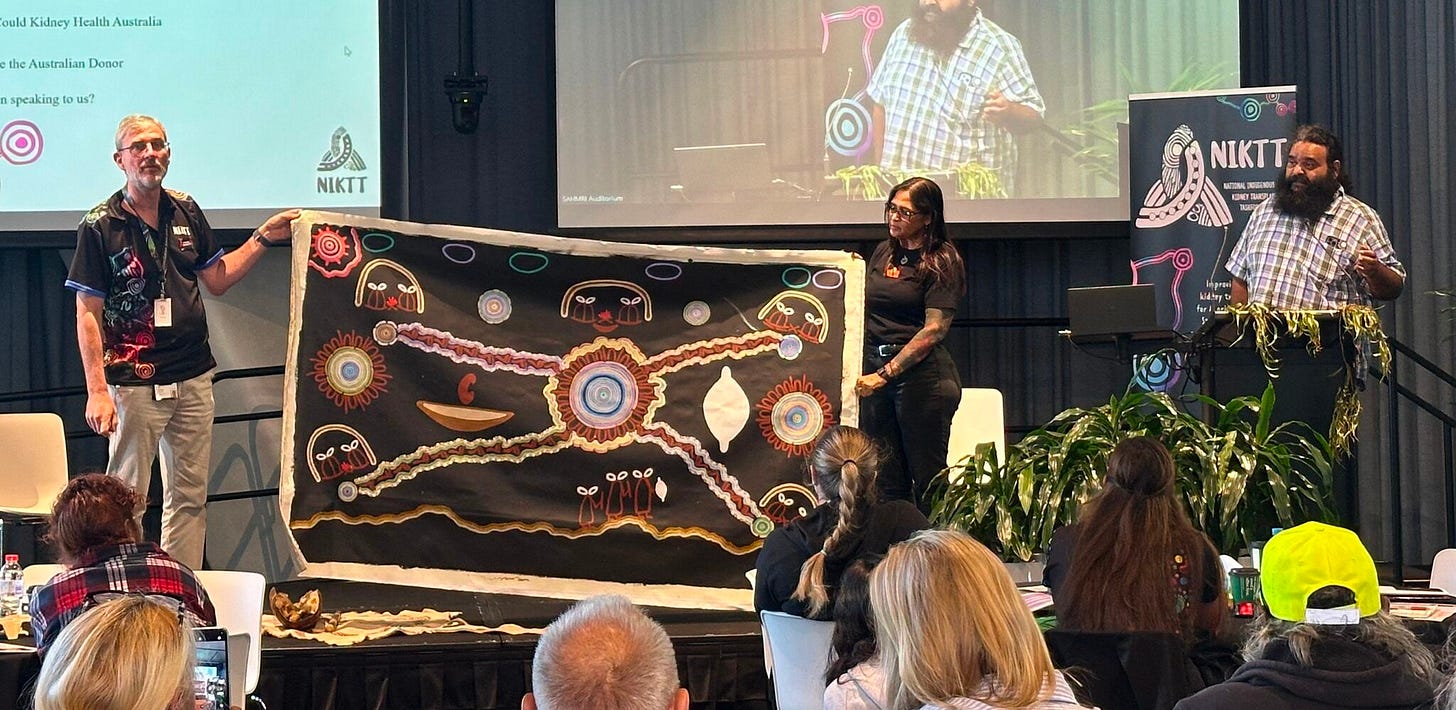
National Indigenous Kidney Transplantation Taskforce (NIKTT) 2025 Gathering – Last week, patient experts, caregivers, clinicians, and community leaders from across Australia met on Kaurna Yarta (Adelaide) to shape the future of Aboriginal and Torres Strait Islander kidney care. (LinkedIn, h/t Isabelle Haklar)
Black History Month Spotlight: Dr. Silas Norman – The American Kidney Fund (AKF) celebrates their Board of Trustees Chair and transplant nephrologist in a recent Q&A. (Kidneyfund.org)
AKHOMM’s series on Black patients with CKD continues – Part 2 featured kidney patient advocate Curtis Warfield, discussing ways to improve healthcare experiences for Black communities. (AKHOMM)
AKF’s Rare Kidney Disease Action Network amplifies patient voices – Hear from Ariana, Jason, and Sherry as they share personal experiences with IgA Nephropathy. (Kidneyfund.org)
Primary care has a funding crisis—this model could help (The Harvard Gazette).
Access Save: A complex case in vascular access care – A 70-year-old ESRD patient with severe arm swelling post-surgery was told further interventions weren’t possible—until a new approach was explored. (LinkedIn, h/t Terry Litchfield)
Jobs
SVP Value-Based Care at Guaranteed
Account Manager (Transplant) - SoCal at Eurofins
Transplant Manager (Remote) at Eurofins
Administrator on Duty (NY) at LiveOnNY
VP, Digital Strategy/Solutions at Fresenius
Regional Home Manager (NY) at DaVita
Senior Director, Digital Health (SF) at Genentech
VP, Healthcare at The Bliss Group
Director, Data Modernization at NNPHI
VP, Population Health at Interwell Health
Palliative APP (Birmingham, AL) at Monogram Health
Head of Brand, Marketing, & Comms at Monogram Health
Sr. Director, Compliance & Privacy at Monogram Health
Thank you for reading our latest biweekly recap on all things kidney health. If you found it valuable, please consider sharing this with 1-2 friends or peers around the Kidneyverse. Thank you!
As a veteran with a service-connected disability, I’ve experienced firsthand how VA claims processing impacts those who have served, and I know dozens of others facing similar struggles due to these decisions. I’ve also built and supported companies that rely on the FDA’s device group, an agency that is now losing critical expertise in AI oversight, safety reviews, and innovation pathways. And in kidney health, these cuts could set back decades of progress, with HRSA, CMS, CMMI, FDA, CDC, and NIH all impacted—agencies that play a vital role in transplantation, care delivery, and research. The stakes are high—and people should understand what’s really at risk.
Two more perspectives worth reading and sharing: Skilled technologists are being forced out of government and Deleting 18F. Also, enjoy Mark Cuban’s response to the 18F firings.
![Signals From [Space]](https://substackcdn.com/image/fetch/w_80,h_80,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F55686857-6b99-45a6-ac0f-09c9f023f2a0_500x500.png)
![Signals From [Space]](https://substackcdn.com/image/fetch/e_trim:10:white/e_trim:10:transparent/h_72,c_limit,f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F4d588ac1-7fac-4bd4-829d-fc7b4e8f1326_1512x288.png)

![Signals From [Space]](https://substackcdn.com/image/fetch/w_36,h_36,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-post-media.s3.amazonaws.com%2Fpublic%2Fimages%2F55686857-6b99-45a6-ac0f-09c9f023f2a0_500x500.png)